The Trauma Recovery Institute
The Trauma Recovery Institute is a leading organisation in treating trauma and trauma based presentations which may manifest in chronic disease, depression, personality disorders, dissociation, ptsd and challenges in functioning in life and loving relationships. The Trauma Recovery Institute offers a number of nervous system based trauma informed therapies, courses, workshops and programs addressing underlying psychological trauma, chronic stress and the presenting symptoms ubiquitous with trauma. Our unique approach is trauma & polyvagal informed neurosequential orientated complex trauma recovery grounded in Interpersonal Neurobiology, an integrative, consilient and coherent blend of bottom up and top down therapeutics delivered through a framework of safety and collaboration helping clients on their journey from reactive survival to receptive secure functioning.
Neurosequential Orientation





Trauma, Chronic stress & PTSD
Trauma is similar to memory cells in the immune system, the brain and nervous system become sensitised to subsequent stressful or perceived stressful events experienced via neuroception as threatening or even life threatening mirroring an original experience or experiences once faced in early childhood. Memory T and B lymphocytes have an essential role in the immunity against microbial pathogens. Immunological memory occurs after a primary immune response against the antigen. Immunological memory is thus created by each individual, after a previous initial exposure, to a potentially dangerous agent. The course of secondary immune response is similar to primary immune response. After the memory B cell recognizes the antigen it presents the peptide: MHC I complex to nearby effector T cells. That leads to activation of these cells and rapid proliferation of cells. After the primary immune response has disappeared, the effector cells of the immune response are eliminated. However, there remain antibodies previously created in the body that represent the humoral component of immunological memory and comprise an important defensive mechanism in subsequent infections. In addition to the formed antibodies in the body there remains a small number of memory T and B cells that make up the cellular component of the immunological memory. They stay in blood circulation in a resting state and at the subsequent encounter with the same antigen these cells are able to respond immediately and eliminate the antigen. Memory cells have a long life and last up to several decades in the body.

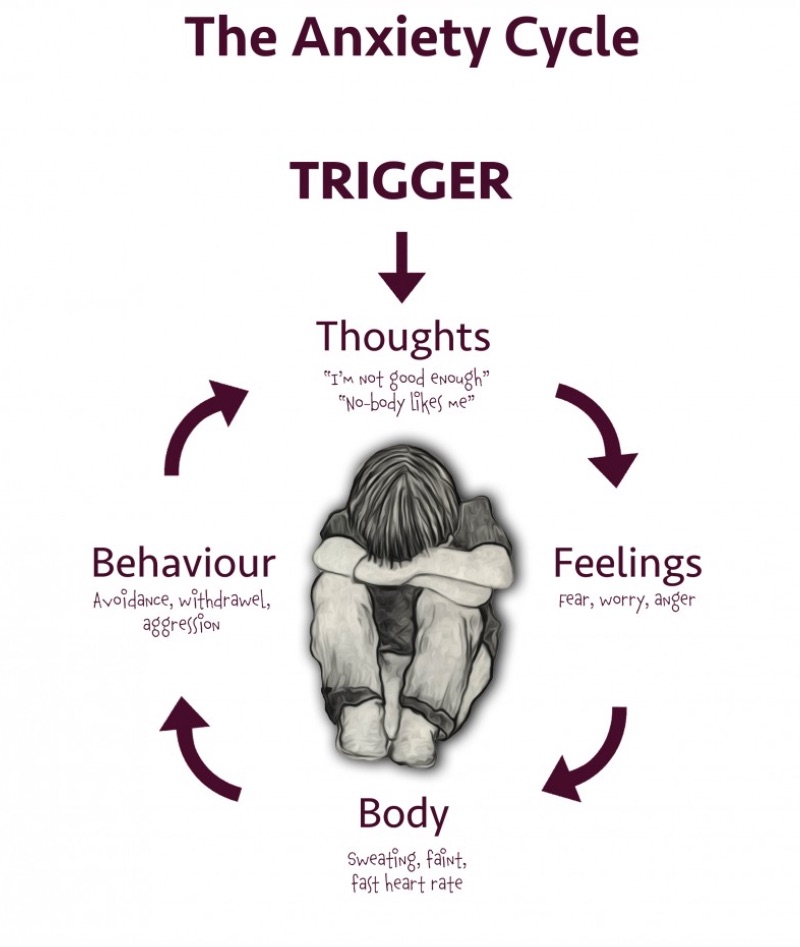
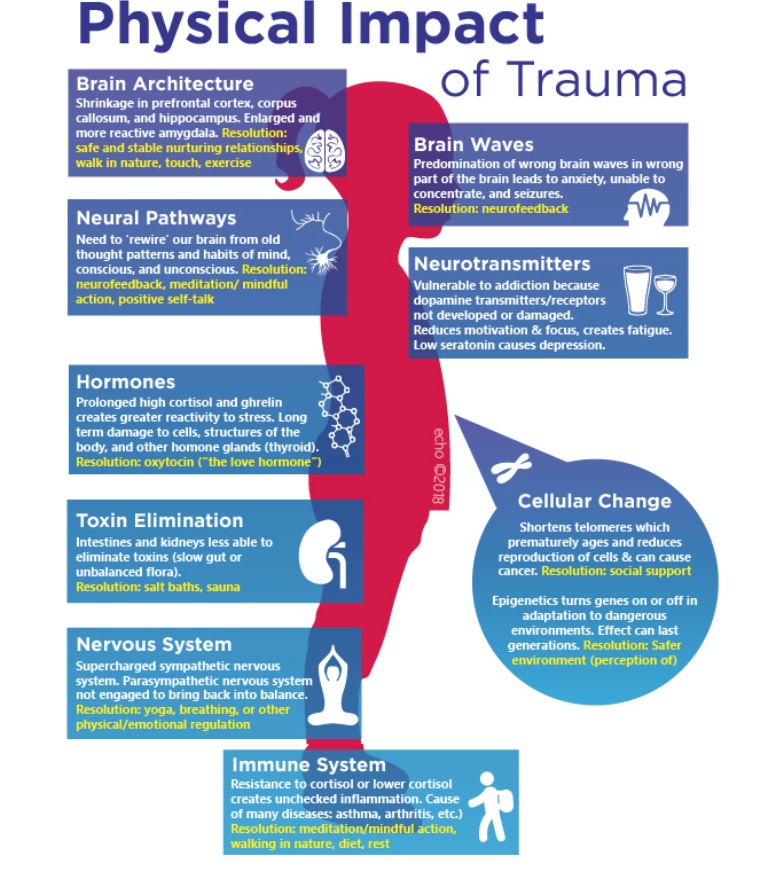
When there has been chronic inflammation, chronic infections or chronic stress/anxiety induced burden on this immune response, these memory cells become overactive and start to attack friendly cells and organs confusing them for threats, this is autoimmunity and presents in syndromes such as IBS, IBD, Colitis etc. The trauma impacted brain and nervous system acts in a very similar way to immune system memory cells responding to subsequent threat or perception of treat which happens below conscious awareness through a process called neuroception. In traumatology this is called sensitised. After a traumatic event or encounter we become sensitised to a look, a sound, a smell, a feeling that may represent a cue of the original event. We then act in ways which may not promote prosocial reciprocity, we may appear defensive, mistrusting, angry, even agressive or withdrawn, all theses are the defenses we use to protect us from a repeat of the original trauma whilst co creating a variation of the original trauma via reenactment. The road to a healthy secure relationship is usually extremely difficult for people who have experienced neglect and trauma precisely because the defenses we use to avoid the painful past often wind up provoking it's recreation in the present setting up a perpetual cycle of toxic stress, inflammation and adversity.
THE POLYVAGAL THEORY
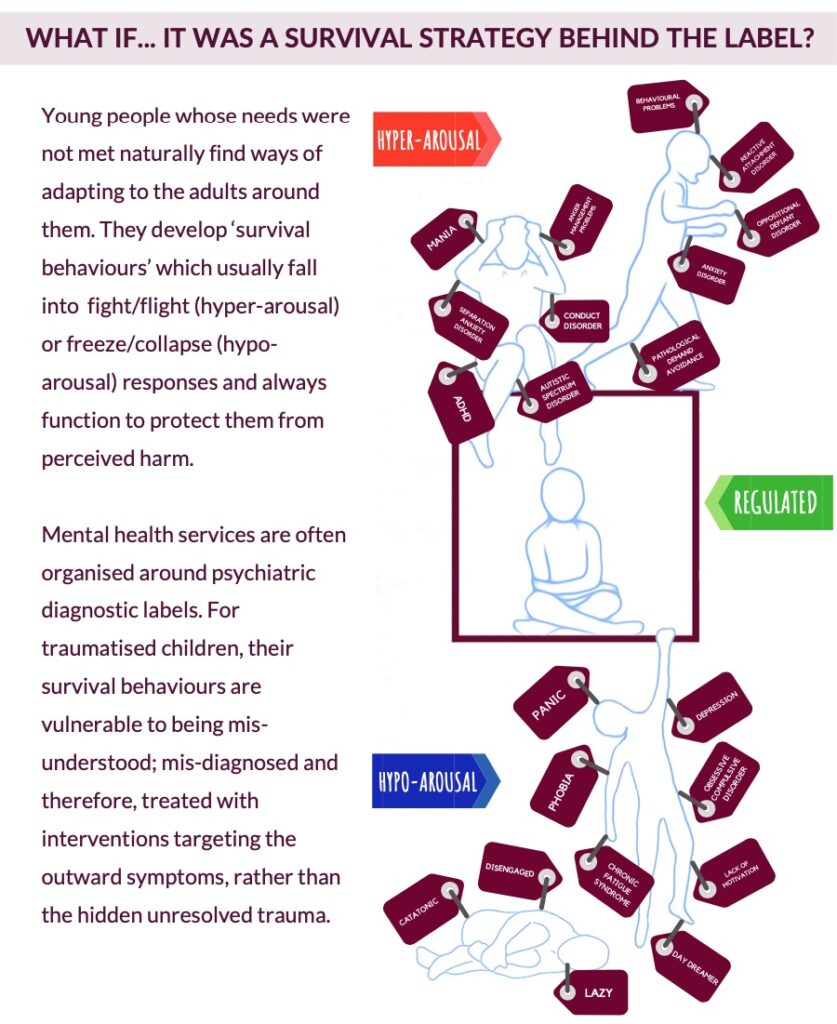
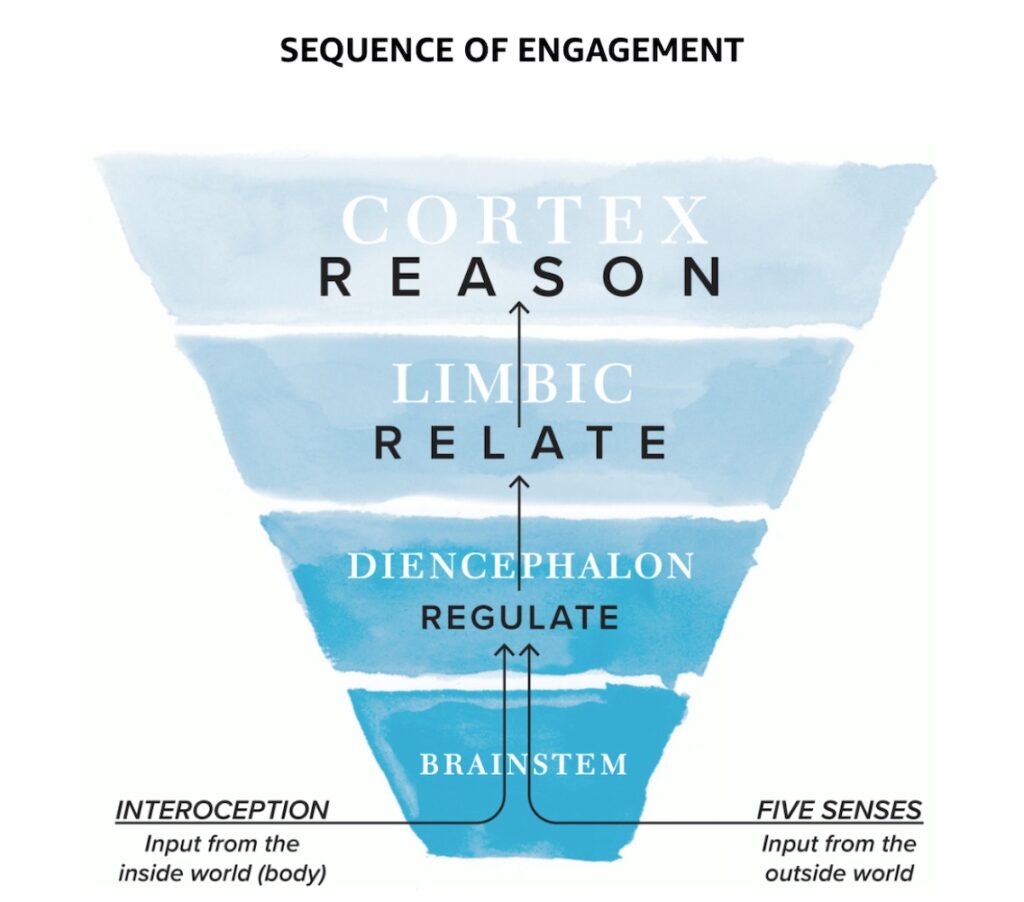
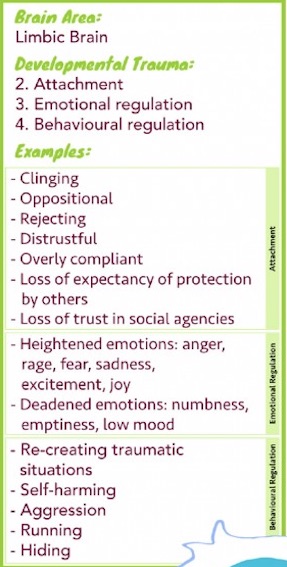
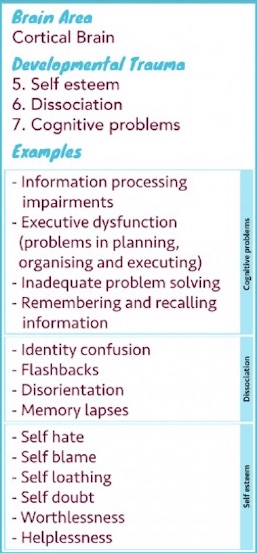
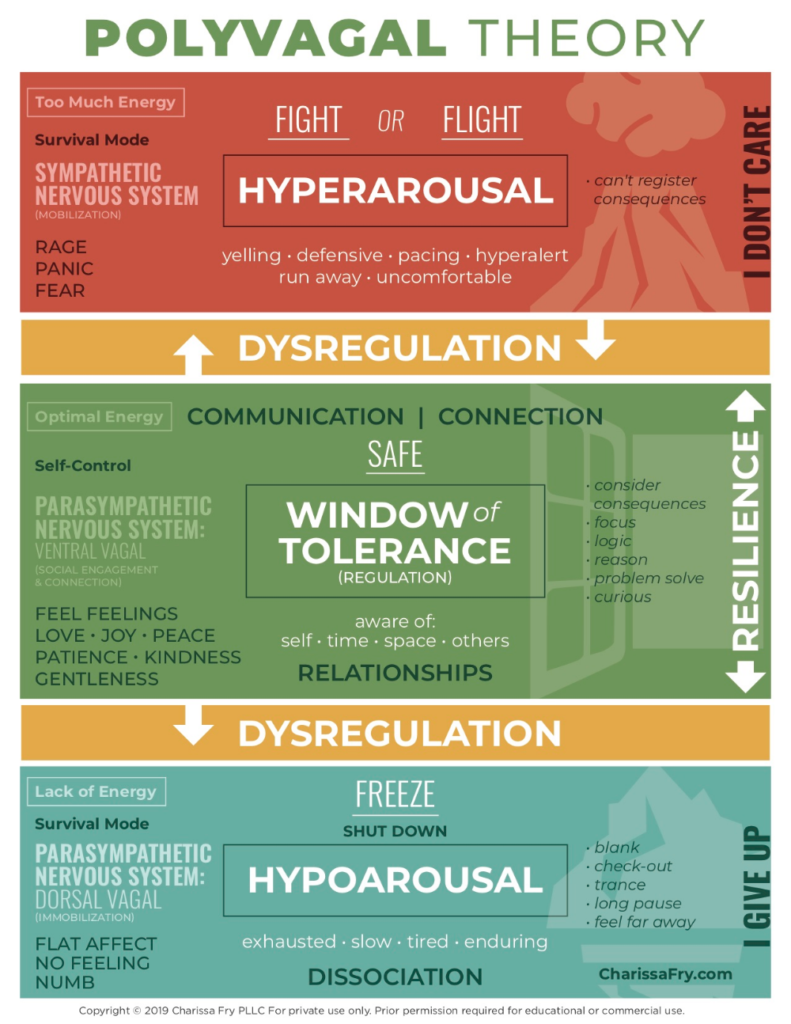
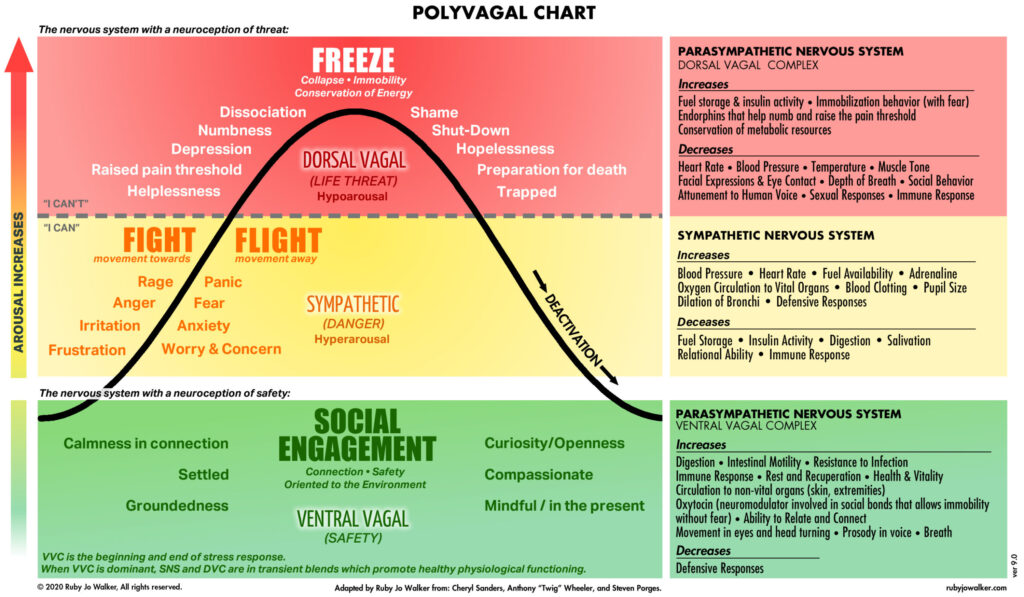
Polyvagal Theory provides a revolutionary map of the nervous system, describing the underlying basis for our behaviour and feelings. The theory proposes that much of our cognitive and emotional intelligence stems from our physical state. Our body has an innate sense of when we are safe and when we are not, and our body responds accordingly by speeding up our heart rate and stress levels if we feel unsafe and have the need to fight or flee— slowing down heart rate and higher brain functions when we are scared to death (“freezing”), or relaxing us and increasing our ability to engage socially and think creatively when we feel safe and appreciated. This internal ‘barometer’ is known as our autonomic nervous system, and Polyvagal Theory sheds new light as to exactly how it works on both individual and social levels. Chronic stress or trauma can prevent our autonomic nervous system from functioning in a healthy way, signalling danger when there is none and keeping us stuck in a state of survival. Social gatherings can be frightening and a simple meeting at work can become threatening. Living in prolonged states of survival often leads to unhealthy adaptive behaviours and significantly increased risks for chronic diseases.
Nervous System Regulation Exercise 1.
Write down What are your “rules of play”? In each of the following categories identify what cues of danger shut down play, what cues of safety support an experience of play, and what beliefs are associated with both the shut down and cues of safety in each category.
- 1. Attunement
- 2. Body Movement
- 3. Object
- 4. Social Interactive
- 5. Imaginative Pretend
- 6. Storytelling
- 7. Creative Fantasy
Understanding Your Nervous System Exercise 2.
Think about when each state ventral, sympathetic and dorsal is most alive and write down with Who, with What, Where and when is each stage of nervous system most alive ?
-
Ventral
( Who, What, Where and When )
-
Sympathetic
( Who, What, Where and When )
-
Dorsal
( Who, What, Where and When )
Understanding Your Nervous System Exercise 3.
In each of the nervous system states ventral, sympathetic and dorsal , write down some words which describe this sate and in each of these states write the following which may speak to an internal belief.
I am .....
The world is ....
MORE POOLYVAGAL EXERCISES
EXERCISE 1 – Recognise
Autonomic awareness is a protective factor. Without the ability to recognise states and state changes, you are at risk for remaining stuck in dysregulation. The question, “Where am I on my autonomic map?” is a simple way to build autonomic awareness.
- Notice. Bring awareness to your autonomic state.
- Name. Stay out of your story and identify your state. Where are you on your autonomic map?
- Repeat these two steps often. Create ease with this practice until you can quickly and accurately place yourself on your autonomic map.
EXERCISE 2 - Reflect
Once the notice-and-name practice becomes easy and automatic, add the next step of turning toward your autonomic nervous system to listen for just a quick moment to what it is telling you. Don't spend a long time hearing the full story.
Just take long enough to get the general idea of what is happening.
- Be curious about what just prompted a mobilization of your sympathetic system, a descent into dorsal vagal conservation mode, or an experience of ventral vagal regulation.
- Listen to what your state wants you to know.
My sympathetic mobilization is telling me...
My dorsal vagal state is letting me know...
My ventral vagal system is inviting me to... - Listen for just a brief moment with curiosity and without judgement. Don't spend more than a minute or so listening.
This practice is a quick experience of listening to the outlines of your story and not diving deeply into the details.
EXERCISE 3 – Playful moments
Playfulness is an important quality that contributes to wellbeing. As you find ways to create opportunities for moments of playfulness, you can become a more playful person and experience the joy and creativity that accompanies play.
- Notice how often, easily, and intensely you engage in a playful experience.
- Increase your playful experiences. Find the ones that bring a smile and the ones that bring energy and play in those ways a little bit more.
- Expand your playfulness. Experiment with experiences in the kinds of play that aren’t in your play repertoire.
EXERCISE 4 – Regulate
Everyday navigation of daily living involves setting goals and then acting to make your goals a reality. Goals are helpful in identifying what you want to achieve and are often stated the form of an intention.
- Consider the autonomic goals you want to set. Ask yourself:
Where do I want my autonomic patterns to take me?
What do I want to change?
What do I want to deepen? - Write goals that address what you discovered. Begin each statement with the words “I intend to.” For example:
I intend to not get stuck in dorsal vagal collapse.
I intend to more quickly manage my sympathetic response.
I intend to find moments of ventral vagal happiness to savor.
Find the words that express your autonomic goals and write your personal intentions.
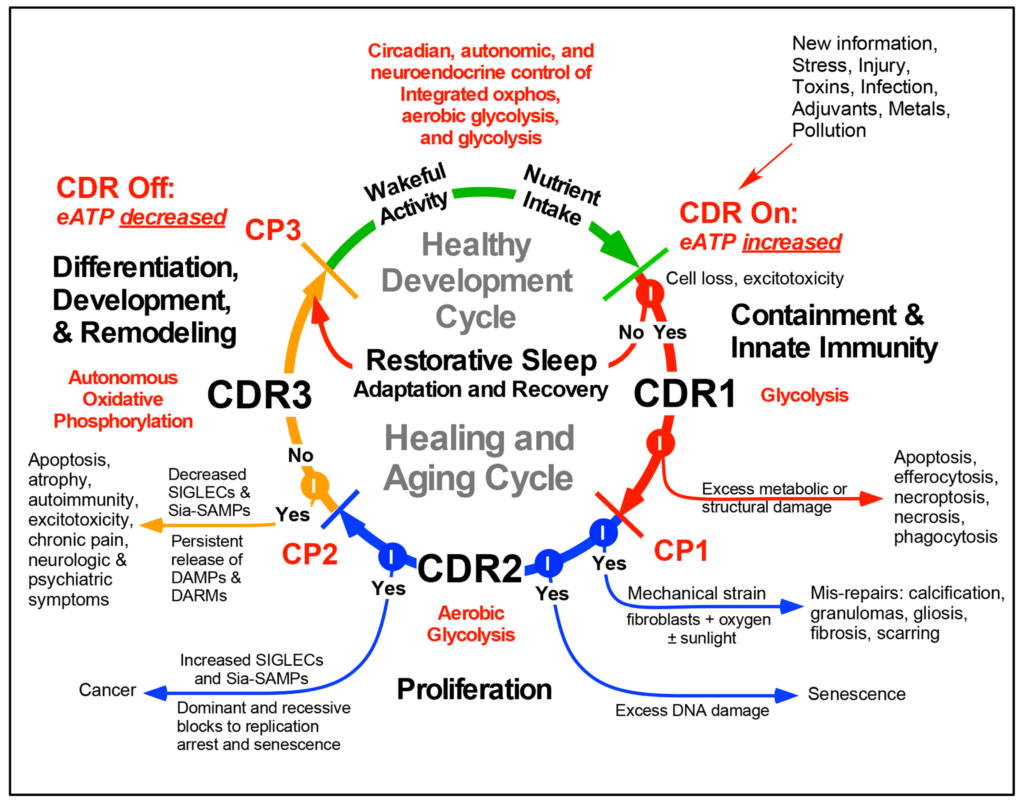
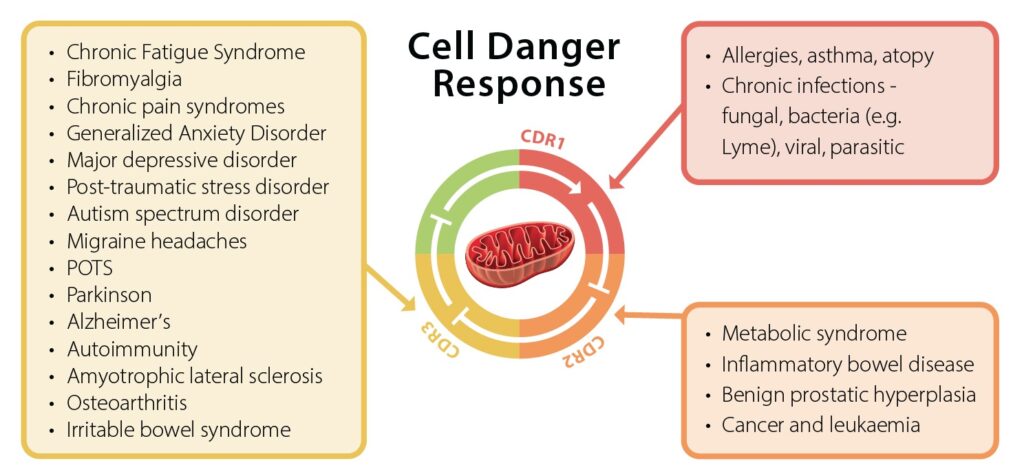
The Cell Danger Response Theory
a biological mechanism of disease
The cell danger response (CDR) is the evolutionarily conserved metabolic response that protects cells and hosts from harm. It is triggered by encounters with chemical, physical, or biological threats that exceed the cellular capacity for homeostasis.
Cell Danger Response
Mitochondria sense and respond to changes in the cellular environment. By sensing safety and danger, mitochondria act as fundamental regulators of the cell danger response (CDR). The CDR is an ancient and universal response to threat, stress, or injury. Mitochondria are uniquely suited to monitor the environmental and genetic conditions, and the gene-environment (ecogenetic) interactions that regulate the CDR. The mitochondrial proteome consists of about 1300 proteins that are transcriptionally and post-translationally regulated according to tissue-specific needs , injury, infection, and presence or absence of environmental pollution. Chemical, physical, and microbial changes that surround all multicellular life on Earth are translated into changes in mitochondrial structure and function. These changes in mitochondria are used to signal safety or danger in the cell, alter gene expression, trigger the healing response, and adjust fitness and susceptibility to chronic illness. These changes even help to adjust the rate of aging in response to environmental stress. The term CDR was originally coined to include all levels of the organismal response to stress, including inflammation, immunity, metabolism, microbiome, epigenetics, behavior and memory. Some aspects of the CDR are studied independently and called the integrated stress response (ISR) and the mitochondrial ISR.
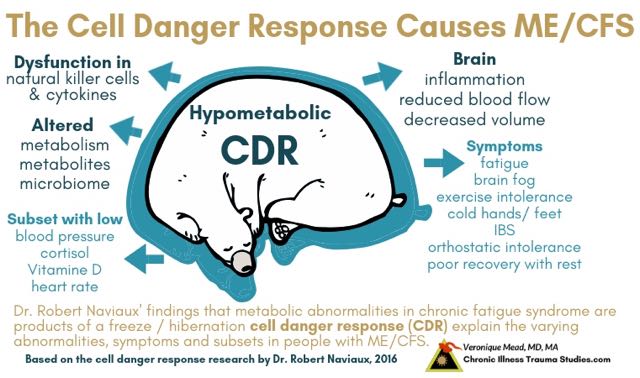
When the CDR is triggered, the priorities of a multicellular organism are reset to optimize survival. The CDR is so fundamental to the survival of all living things, that the same core defenses of metabolism, inflammation, immunity, microbiome, brain function, sleep pattern and behavioral changes are activated by many different kinds of threats. These threats can be as diverse as an infection, poisoning, physical, or psychological trauma, and still trigger the same stereotyped sickness behavior. This stereotyped response to danger includes withdrawal from social contact, activation of innate immunity, decreased speech, fragmented sleep, head, muscle and abdominal aches, changes in the gut microbiome, and the increased sensitivity to touch, sound, and light that many people experience when they have the flu, or are recovering from a serious injury. It is the CDR that produces these familiar signs and symptoms. At a cellular level, the cell danger response cannot be turned off until the cell receives the final “all clear” signal. Until then, the CDR remains stuck in a repeating loop that blocks further healing in an attempt to eradicate perceived danger. This can lead to long-term suffering, disability and chronic disease. Only when a cell perceives safety can it heal completely.
The concepts of cellular perception and reactivity are critical. Danger can be real or imagined. From the time we take our first breath, our genes are hard-wired to treat the world as a dangerous place, to anticipate a struggle to survive. When conditions become extreme, one cell can defend itself with powerful chemical weapons, while another may sacrifice itself to save its neighbors by activating a single-cell “self-destruct” sequence. The threshold for cellular reactivity is set by past environmental experience. The perception of safety leads to calm. Perception of danger leads to hypersensitivity.
Cell Danger Response
Chronic Pain Syndrome
Most medical treatments for chronic pain fail. That’s because pain isn't a purely medical issue – it's also cognitive, emotional and environmental. This means that effective treatments must target the brain in addition to the body.
Central sensitization refers to the amplification of pain by central nervous system mechanisms. Classically described as a consequence of ongoing nociceptive input, it is increasingly recognized that central sensitization also occurs independent of peripheral injury or inflammation. Features of central sensitization have been identified in nearly all chronic pain conditions, and it is considered the primary underlying cause of pain in conditions such as fibromyalgia. Central sensitization is characterized in these condi- tions by widespread pain and multisite hyperalgesia/ allodynia. Co-occurring symptoms include fatigue, mood and cognitive problems, sleep disturbances, and multisensory hypersensitivity. Individuals with central sensitization often report previous exposure to psychosocial or physical stressors, and a higher personal lifetime and family history of pain, with the latter findings supported by genetic studies. Neuroimaging studies of central sensitization show evidence of: changes in brain gray matter in pain processing regions; neurochemical imbalances; and altered resting brain-network connectivity between pronociceptive and antinociceptive brain areas. Immune system abnormalities have also been demonstrated in individuals with centralsensitization. The recognition of central sensitization, and whether it is being driven by ongoing nociceptive input or it is occurring in the absence of a peripheral driver, is critical for effective pain management.
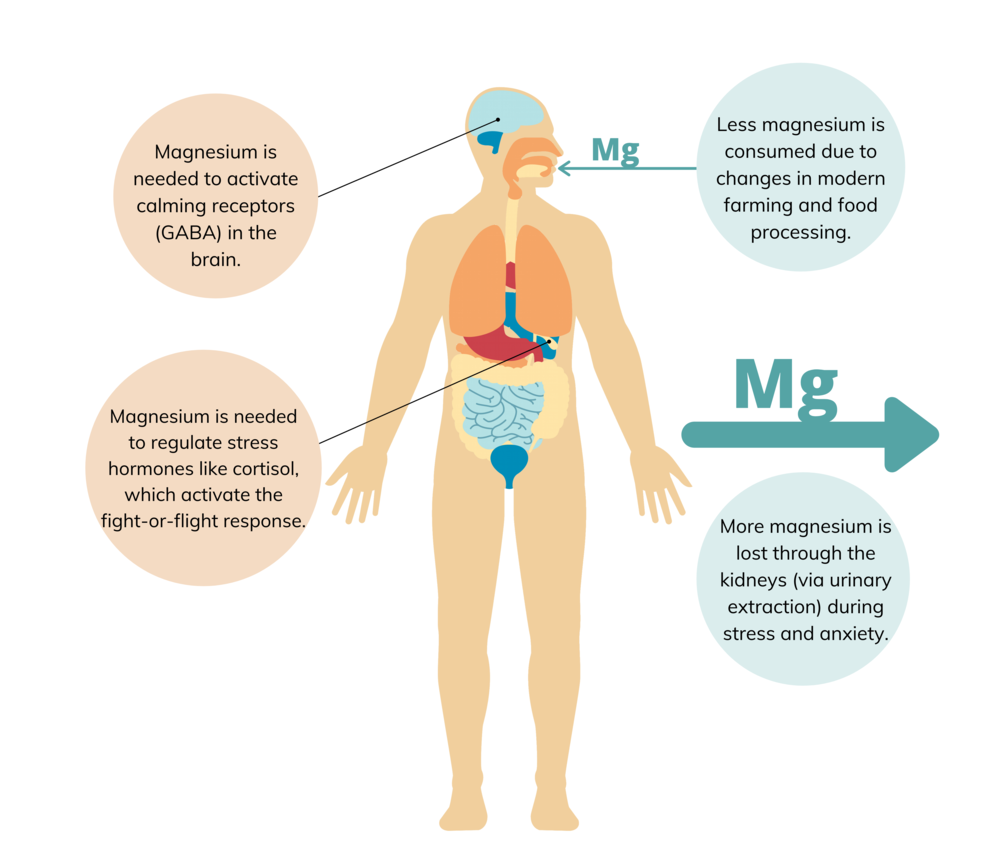
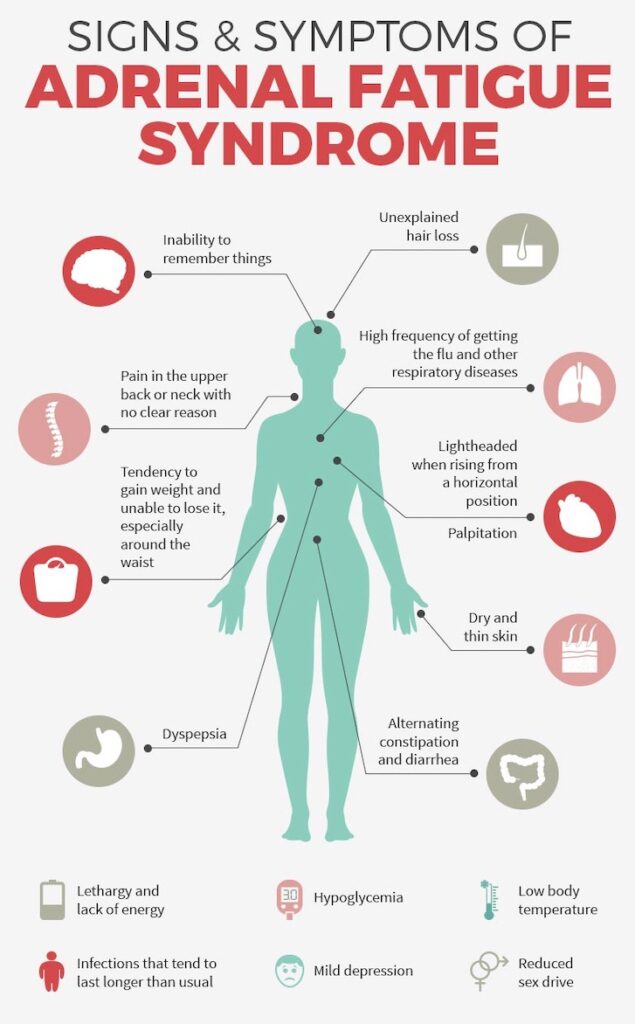
HPA Axis Regulation: Trauma Adaptation & Hidden wounds
Chronic psychosocial stress has adverse effects on the physical and mental health of individuals and organizational effectiveness. Biological responses to stress promote adaptation, maintenance of homeostasis, and survival (“allostasis”) via neuroendocrine, cardiovascular, autonomic, immune, and metabolic systems. However, chronic stress leads to long-term dysregulations in these systems (“allostatic load”) that can promote and exacerbate pathophysiology. Individuals under prolonged response to chronic emotional and interpersonal stressors and insufficient down regulation of the stress response are at high risk of developing long-term symptomology such as autoimmune disorders. The brain is the key organ for the stress response. Exposure to stress causes the activation of the sympathetic–adrenal–medullary (SAM) axis, resulting in the release of epinephrine and norepinephrine, which affect the heart rate and other autonomic changes, as well as the hypothalamus–pituitary–adrenal (HPA) axis, leading to the release of glucocorticoids such as cortisol. During chronic stress, prolonged and repeated activation of the HPA axis occurs as an adaptive mechanism to stress. This increased HPA axis activation can result in hypercortisolism. High cortisol concentrations play an important role in various psychoneuroendocrinological processes and hypertension. Insulin resistance, hyperglycemia, inflammation, visceral fat accumulation, and the metabolic syndrome are the consequences. A state of hypofunctioning with related hypocortisolism can follow. Furthermore, chronic stress leads to hyperactivity of the sympathetic nervous system. Possible related risks include increased heart rate, activation of the renin–angiotensin system, and oxidative stress causing chronic inflammation. The mesolimbic dopaminergic system and other brain regions involved in stress/motivation circuits may play important roles in chronic stress-induced food intake, food preference and reward sensitivity. However, uncontrollable chronic stress exposure can lead to poor dietary choices, weight gain, diet-related metabolic risk, and increased specific nutrient requirements. An adequate supply of specific amino acids, as a precursor for neurotransmitters, is suggested to positively influence the stress-induced imbalance between excitatory (e.g., norepinephrine, dopamine, and glutamate) and inhibitory (e.g., serotonin, gamma-aminobutyric acid (GABA), and glycine) neurotransmitters and neurological, emotional and behavioral consequences. Consuming the amino acid tyrosine, a precursor for dopamine and norepinephrine, is considered an effective cognition enhancer, when neurotransmitter function is intact and dopamine and/or norepinephrine are temporarily depleted. Taurine plays a role in the central nervous system, in antioxidant and anti-inflammatory actions, and in several metabolic processes. Taurine acts as an inhibitory neuromodulator, as a cytoprotectant against stress-related neuronal damage, and is commonly known for its claimed energizing properties and anti-fatigue compound. Low brain serotonin concentrations are associated with poor memory and depressed mood. Cerebral serotonin is synthesized from l-tryptophan (l-Trp) with the rate limiting step being catalyzed by the enzyme tryptophan hydroxylase. The precursor l-Trp is transported across the blood–brain barrier. Several amino acids, the branched-chain amino acids (BCAA, such as l-leucine, l-isoleucine, and l-valine), and the aromatic l-tyrosine and l-phenylalanine, collectively known as the competing amino acids (CAA), are transported via the same carrier system. Studies have shown that an increased plasma ratio of free l-Trp to the sum of CAA results in an uptake of l-Trp by the brain, suggesting that this condition may increase the synthesis of serotonin. l-ornithine supplementation has shown potential to relieve stress, reduce HPA axis activity, and improve fatigue-related sleep quality. Moreover, water-soluble vitamins, particularly B-vitamins and vitamin C, together with minerals, such as magnesium and zinc, act as cofactors in the synthesis and metabolism of neurotransmitters. Therefore, these micronutrients are essential for regulating the stress response. An adequate intake of all eight B vitamins is essential for optimal physiological and neurological functioning. Folate, B6, and B12 are directly involved in neurotransmitter synthesis and homocysteine metabolism. Vitamin C, a key antioxidant of the central nervous system, is involved in neuromodulation, -protection, and transmission. Zinc and magnesium are essential for adequate functioning of the neurotransmitter systems and exhibit antidepressant properties. Individuals who are exposed to a stressful lifestyle and chromic stressors are at risk of marginal deficiencies of one or more of these micronutrients.
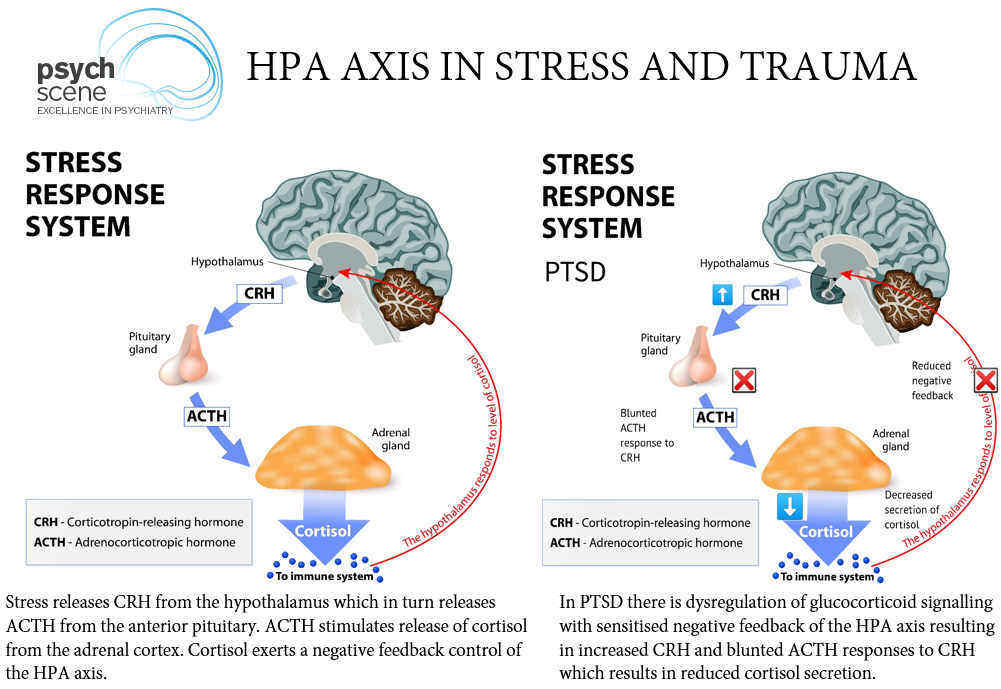
Cortisol and the Diseases of Stress: The Price of Adaptation
Stress basically demands that the brain and body adapt to a stressor—an event or experience that disrupts homeostasis but is not sufficient to trigger the full-blown fight/flight response. There’s an element of arousal in this process, though not as extreme as that in the fight/flight response, and the amygdala is mildly activated when the brain senses messages that imply even a subtle threat. There is a continuum between stress and trauma that is mainly defined by the degree of helplessness the person is experiencing. In fact, the escalation of a stressor to actually being a life threat is entirely possible. But if the stressor continues without ever becoming a life threat, the brain takes a different pathway than it does in trauma to adapt. This pathway is basically the same as the sympathetic nervous systems relationship to the hypothalamic-pituitary-adrenal (HPA) axis. The HPA axis is the origin of the hormonal response by the body’s endocrine system to prepare the body to adapt to a stressor as long as it persists. The end result is the release of cortisol from the adrenal cortex, or outer layer of the adrenal gland. Cortisol damages the neurons of the hippocampus and can contribute to memory and cognitive problems in trauma victims. In large amounts, it may also affect the cerebral cortex, producing arousal, vigilance, delusions, anxiety, rage, and even psychosis. As long as the stressor remains present, cortisol will remain elevated in order to help the body deal with the ongoing, low-grade threat. This state of threat will result in the gradual development of the GAS. Helping us maintain vigilance in the face of low-grade threat, the GAS state of autonomic tuning promotes the ability of our heart and circulatory system to deal with increased physical demands and our level of blood glucose to meet the increased caloric energy demands of the body and especially the brain. In the relatively short term, it promotes survival, but in the longer term it literally causes a breakdown of the body. Cortisol also acts as a modulator of the immune system. In high amounts, it suppresses the immune system. In the early days of organ transplantation, chemicals related to cortisol were used to suppress the immune system to prevent organ rejection. Cortisol-related drugs have also been used in autoimmune diseases, such as rheumatoid arthritis, lupus, and multiple sclerosis. Autoimmune diseases are inflammatory in nature, and cortisol also suppresses inflammation. But improvement in the autoimmune diseases with cortisol is associated with the destructive effects of the GAS.
Suppression of the immune system unfortunately also makes the person more prone to what are called “opportunistic” infections by bacteria and viruses that aren’t normally very infectious. If taken for a lengthy period of time, cortisol also can contribute to the development of unusual forms of cancer that are generally held in check by the immune system. In many ways, prolonged exposure to cortisol leaves the person subject to many of the tumors and infections seen in the immune deficiency caused by the AIDS virus. As a result, during prolonged stress, persons are vulnerable to the development of viral diseases. That’s why cold sores are common under stress. Cortisol also causes the kidneys to reduce their excretion of salt in the urine. Retaining salt causes blood volume to increase, an important piece of survival insurance in case the threat becomes physical and the person experiences injuries causing a loss of blood. Increased blood volume also guarantees the brain’s access to circulation. Both of these effects are adaptive measures for dealing with stress in the short term. Cortisol also raises blood pressure, during both exertion and rest, and increases baseline pulse rate, both of which ensure maximal blood flow to the brain. It causes a significant increase in blood glucose levels. The brain counts solely on glucose as a source of energy. Increased vigilance, glucose, blood pressure, pulse, and blood volume help provide support for blood circulation and optimal oxygen and nutrients for brain function—in the short term. But cortisol also causes an increase in serum cholesterol and other lipids. It causes an increase in secretion of stomach acid. You are probably beginning to see the price exerted by the adaptive GAS. Elevated blood pressure may contribute to sustained hypertension and stroke. Sustained elevated blood sugar may trigger clinical diabetes. Elevated blood lipids may lead to atherosclerosis and coronary artery disease. Immune suppression may lead to opportunistic infections and conceivably cancer. Elevated stomach-acid secretion may lead to peptic ulcers. Increased vigilance can lead to mental disorders, especially mania and psychosis. Finally, cortisol in the long run is catabolic—it breaks down and changes tissues. It causes wasting of muscles, increased fat deposition about the abdomen, osteoporosis, swelling of the face, and the masculine effects of acne and increased facial hair growth in both genders. Many of these conditions have been called “the diseases of stress,” and, in fact, this is partly true. During the early stages of recovery from serious injuries, many of my rehabilitation patients manifested some of these conditions, especially hypertension, acne, cold sores, weight gain, and hypervigilance. Usually these conditions spontaneously subside with time. But if prolonged, the adaptive GAS comes at considerable cost to the brain and body. Unfortunately the burden of the GAS may not always subside, progressing instead to the diseases and syndromes of trauma. The element of helplessness in an ongoing stressful situation may grow with the passage of time. The burden of financial loss, litigation, impairment of human relationships, and increasing social isolation may cause a shift in brain and body physiology. In this context, a significant number of my injured patients went on to develop what I’ve called the diseases of trauma, syndromes increasingly at the parasympathetic end of the spectrum of autonomic dysfunction.
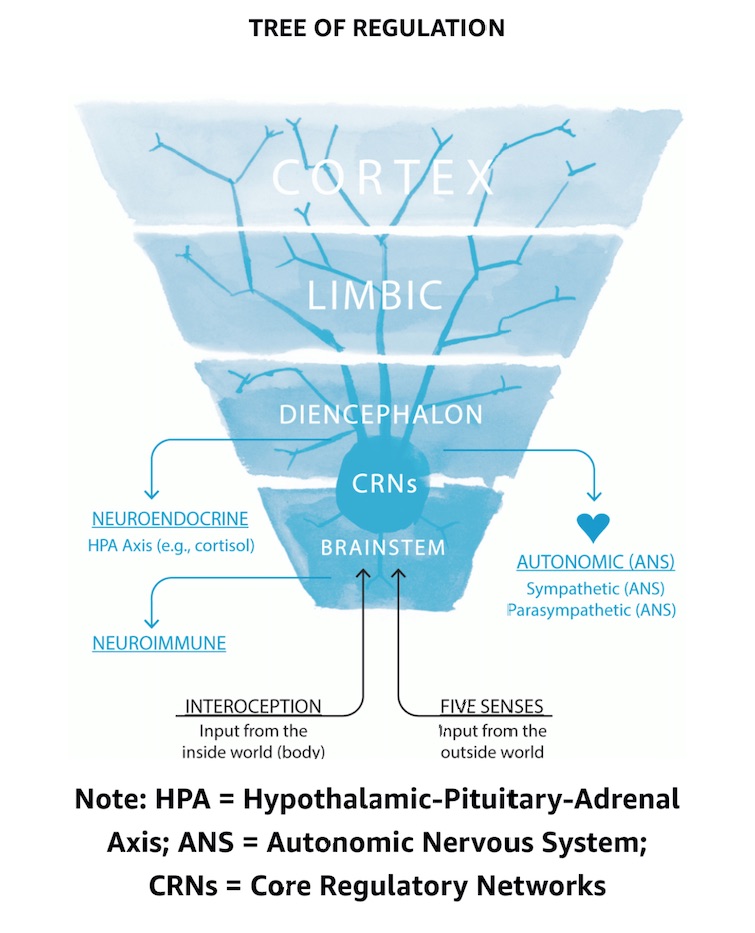
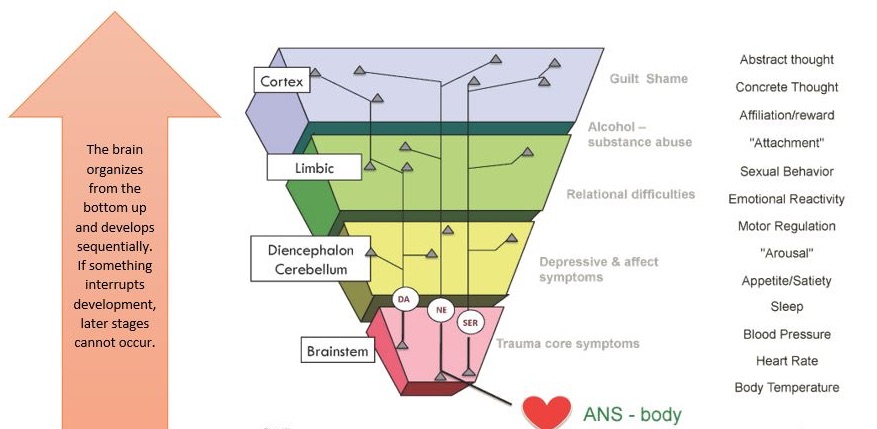
the neurophysiology of threat and trauma
the neurophysiology of threat and trauma The frontal and central areas of the right cerebral hemisphere are the regions in the brain which attend to the arousal response and to threatening information. The parts of the brain that function in an executive fashion (e.g. thinking, planning, communicating, using any type of rational thought) are, in general, not essential for the execution of emergency behavior. Typically, the first level of information that warns us of an impending threat is accessed and received by the primary senses (smell, vision and hearing). Messages from these basic senses are routed to the locus ceruleus or blue center - a tiny cluster of cells in the brainstem. The locus ceruleus sends the message on the the amygdala (the ‘olive’) which is the center for memory of emotionally laden information. Because of its function as the storehouse and processor of emotionally charged experiences, the amygdala plays a crucial role in the mediation of the response to a perceived / conditioned threat experience. Therefore, any part of the brain receiving information which has been processed by the amygdala is likely to be influenced significantly by the emotional conditioning attached to the threat experience. The amygdala then sends messages tot the hippocampus (the ‘sea horse’), as well as to other parts of the brain. The hippocampus forms a conscious structure for the threat-based message that includes its emotional / conditioned importance, and then sends it on to the orbitofrontal cortex, the master regulator of survival behavior (both conscious and unconscious). The orbitofrontal cortex then sends information to many parts of the brain which may then organize and initiate the necessary behavior patterns which can help the individual survive. It also activates the body’s endocrine response through the hypothalamic / pituitary / adrenal (HPA) axis. The hypothalamus is a center deep in the middle and base of the brain. In addition to regulating many other complex functions (e.g. sleep and appetite), it also regulates the autonomic nervous system. In the case of a threat, the sympathetic nervous system (the energy-burning survival part) is activated. The pituitary gland (the master endocrine gland) is also activated and initiates the body’s endocrine response. The pituitary gland, through the hormone adrenocorticotropic homone (ACTH) stimulates the adrenal glands to release cortisol, which puts a brake on norepinephrine - thus modulating the brain’s arousal response.In the event that the individual survives the immediate threat, cortisol also prepares the animal to manage ongoing stress through changes in its circulation, metabolism, and immune responses. This complex interaction of nerve centers, glands, and chemicals is typical of the multiple interactive feedback systems by which the body is designed to not only survive a threatening event, but also to regulate itself and to promote stability of the entire organism.
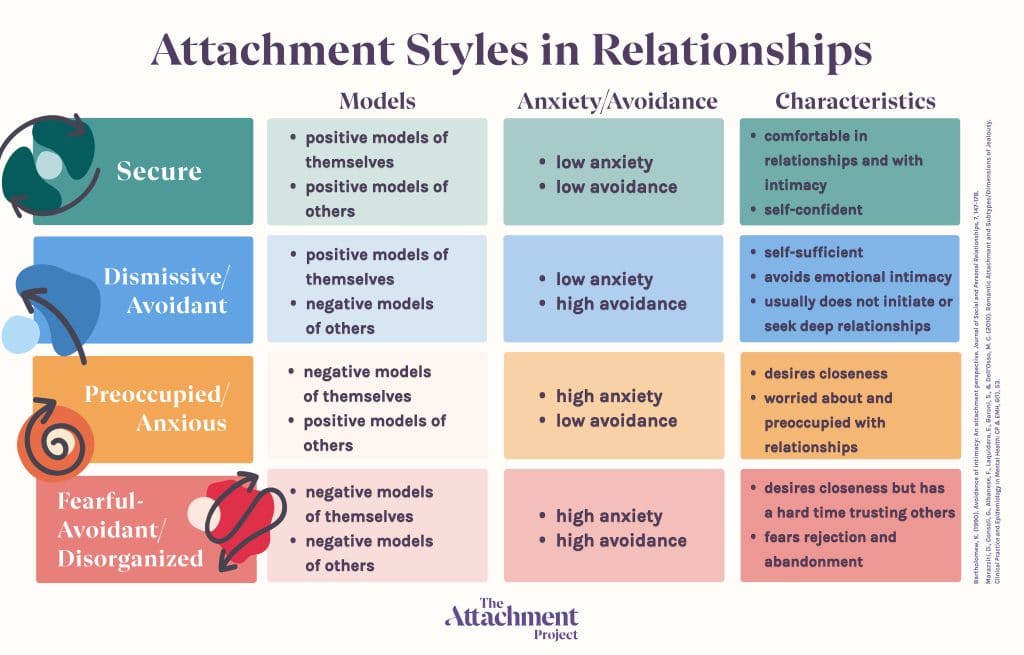
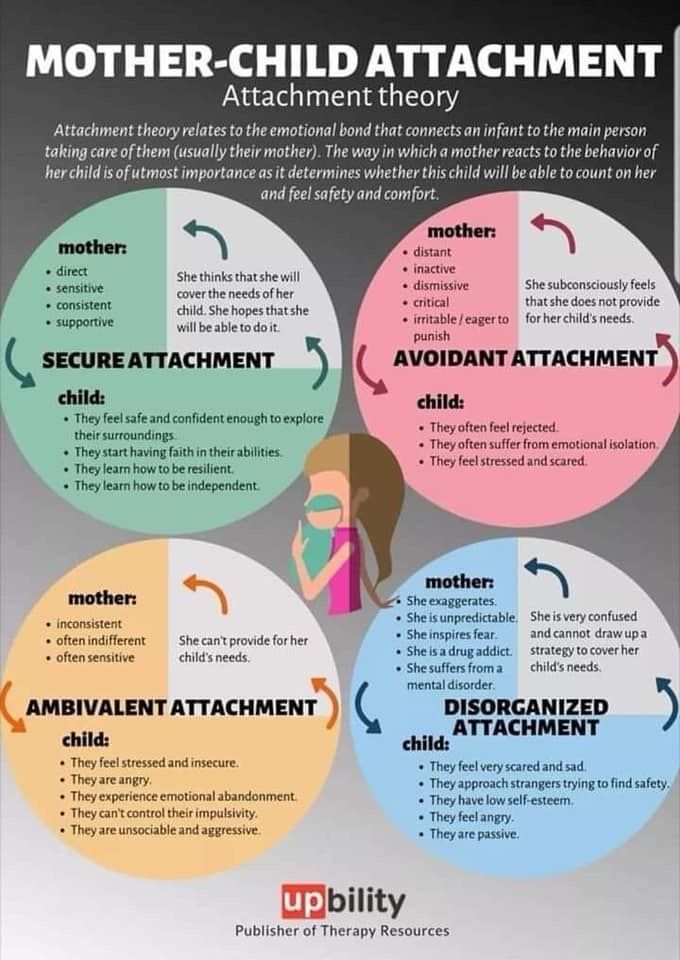
attachment research & principle
Attachment is defined as a “lasting psychological connectedness between human beings” (Bowlby, 1969). Our experiences as children with our primary caregivers inform our attachment blueprint which determines how we engage or disengage with relationships as adults. Attachment theory is essentially a regulatory theory, and attachment can be dened as the interactive regulation of biological synchronicity between organisms. This model suggests that future directions of attachment research should focus upon the early-forming psychoneurobiological mechanisms that mediate both adaptive and maladaptive regulatory processes.
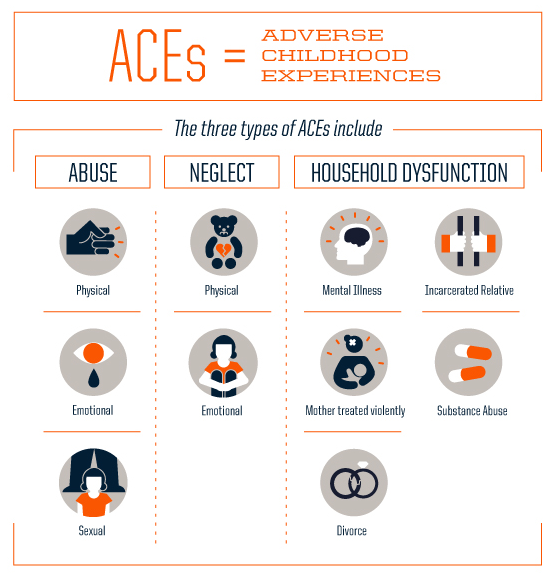
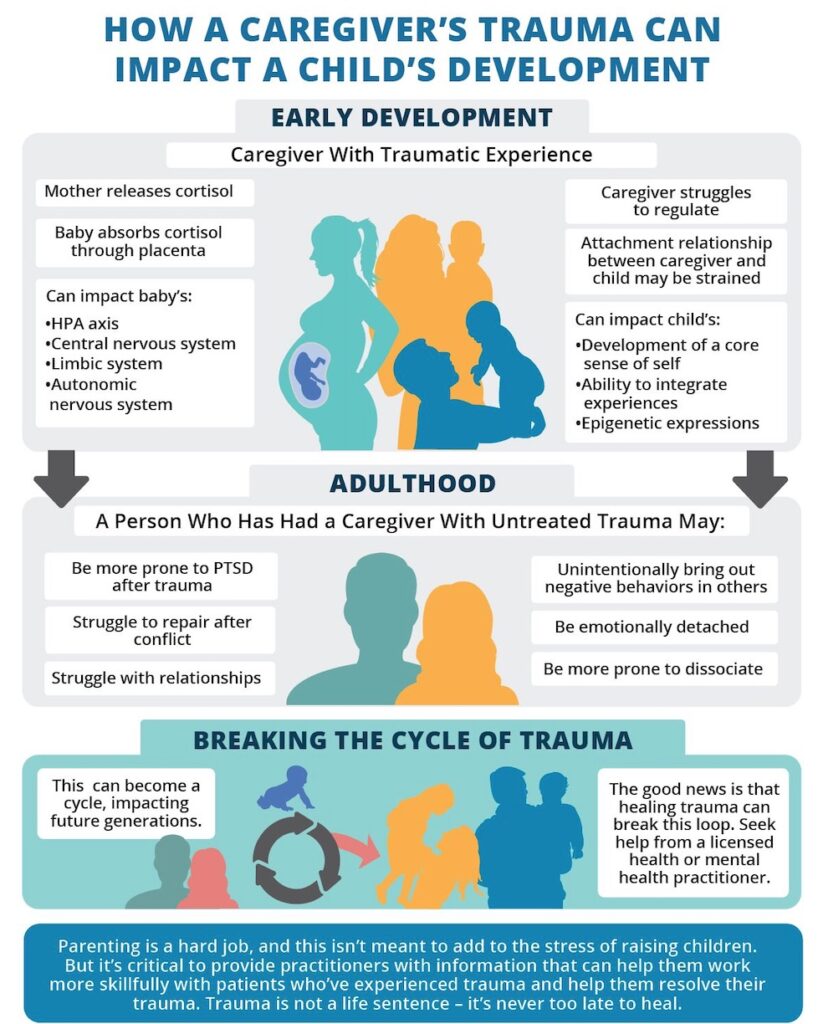
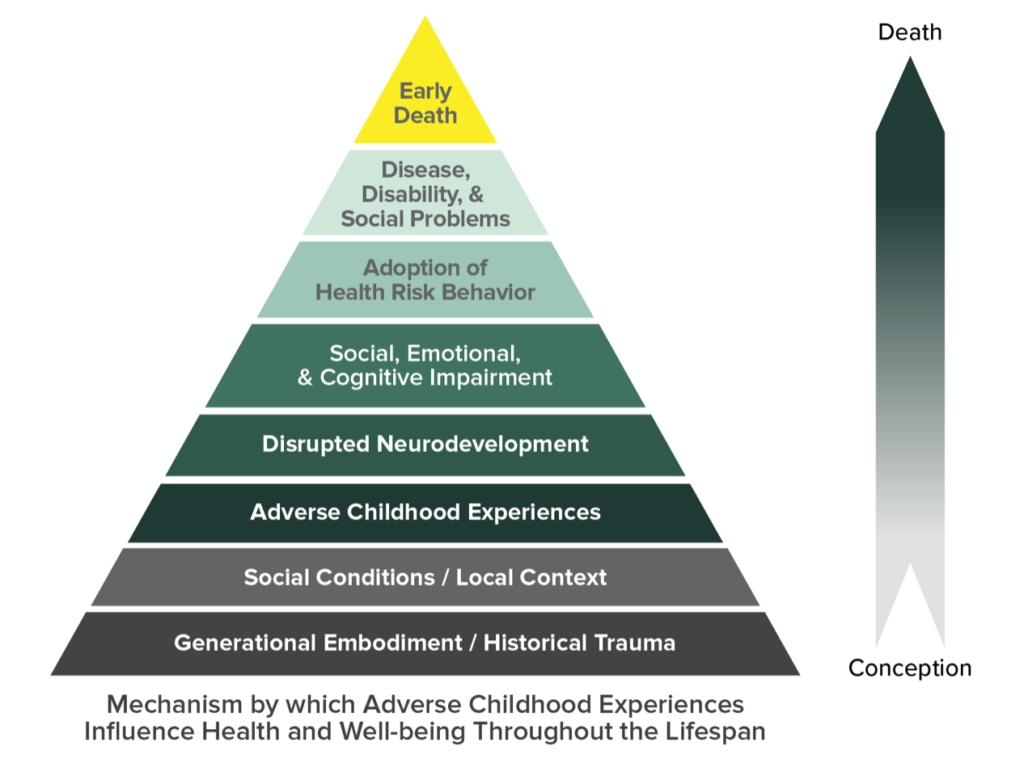
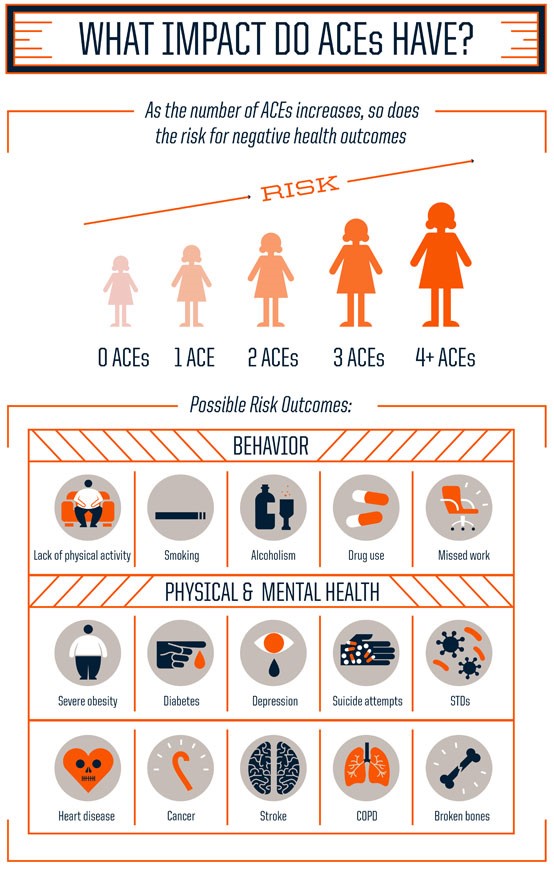
adverse childhood experiences
Adverse childhood experiences (ACEs) can have a tremendous impact on future violence victimization and perpetration, and lifelong health and opportunity. Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years). For example:
- experiencing violence, abuse, or neglect
- witnessing violence in the home or community
- having a family member attempt or die by suicide
- Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding, such as growing up in a household with:
- substance use problems
- mental health problems
- instability due to parental separation or household members being in jail or prison
- Lack of attunement
- Unmet emotional needs
- Physical, sexual and emotional abuse
ACEs are linked to chronic health problems, mental illness, and substance use problems in adulthood. ACEs can also negatively impact education, job opportunities, and earning potential. However, ACEs can be prevented. Please note the examples above are not meant to be a complete list of adverse experiences. There are many other traumatic experiences that could impact health and wellbeing.
neglect and complex trauma
proximal abandonment
The great child psychiatrist, D.W. Winnicott, once pointed out that two things can go wrong in childhood that may adversely affect development: When things happen that shouldn’t happen (e.g., trauma), and when things do not happen that should happen. This latter refers not to overt trauma, but to the stresses and distractions that keep many parents from offering their children the attuned, emotionally present interactions that optimal brain- and personality development require. Many children are being negatively affected in this way, even if not formally traumatized. Emotional or proximal abandonment in childhood can happen if the primary caretaker, usually the mother, is unable to be present emotionally for her baby. It’s often because she’s replicating her childhood experience, but it may also be due to stress. It’s important for a baby’s emotional development that the mother attune to her child’s feelings and needs and reflect them back. She may be preoccupied, cold, or unable to empathize with her child’s success or upsetting emotions. He or she then ends up feeling alone, rejected, or deflated. The reverse is also true – where a parent gives a child a lot of attention, but isn’t attuned to what the child actually needs. The child’s needs hence go unmet, which is a form of abandonment.
This form of abuse and neglect can lead to complex trauma. It by its nature is very pernicious often showing up as confusion in the clinical setting with clients often sharing to the therapist," I don't understand why I feel like this, my parents were good people and they were always there for me, they supported me and were mostly present my entire childhood". This confusion leads to shame spirals, self blame and criticism represented by an internal dialogue such as " I feel like this because I am useless, worthless or no good".
innerchild research & principle
covert incest or emotional incest research
Covert incest occurs when a child becomes the object of a parent’s affection, love, passion, and preoccupation. The parent, motivated by the loneliness and emptiness created by a chronically troubled marriage or relationship, makes the child a surrogate partner. The boundary between caring and incestuous love is crossed when the child exists to meet the needs of the parent rather than the child. The term Emotional Incest (also known as covert incest or psychic incest) describes a relationship between parents and children that is sexualized, without actual incest/sexual contact. The relationships are harmful and one-sided, and similar to a relationship between adult sexual partners but without the type of physical contact that would qualify it as child sexual abuse. The effects are similar to, though less severe, than that of actual incest. The definition of Emotional Incest has a broad set of criteria. Basically, Emotional Incest, is a covert incest, a form of emotional abuse in which the relationship between a parent and a child is inappropriately sexualized without actual sexual contact. Often substance abuse, as seen through the alcoholic dependent needy dysfunctional parent for instance, is associated with covert incest. The effects of this covert incest somewhat mimic sexual incest but often to a lesser degree. The victims have been described as having anger or guilt towards parents and issues with self-esteem, addiction and sexual and emotional intimacy
Emotional Incest started to be recognized about 25 or 30 years ago. It has primarily been defined by the few researchers and therapists who acknowledge it and work with it, as as an emotionally abusive relationship between a parent (or step-parent) and child that does not involve incest or sexual intercourse. It involves similar interpersonal dynamics much like the relationship between sexual partners. Emotional Incest rears up when a parent is unable or unwilling to maintain a relationship, healthy or otherwise, with another adult and forces the emotional role of a spouse onto their child instead. The child’s needs are ignored and instead the relationship exists primarily to meet the needs of the parent. The adult usually is not aware of the issues and implications created by their actions, and justifies the relationship in a variety of ways. Emotional incest happens when parents fill their own inner emptiness by overly connecting with their child, bonding as equals and “buds”.
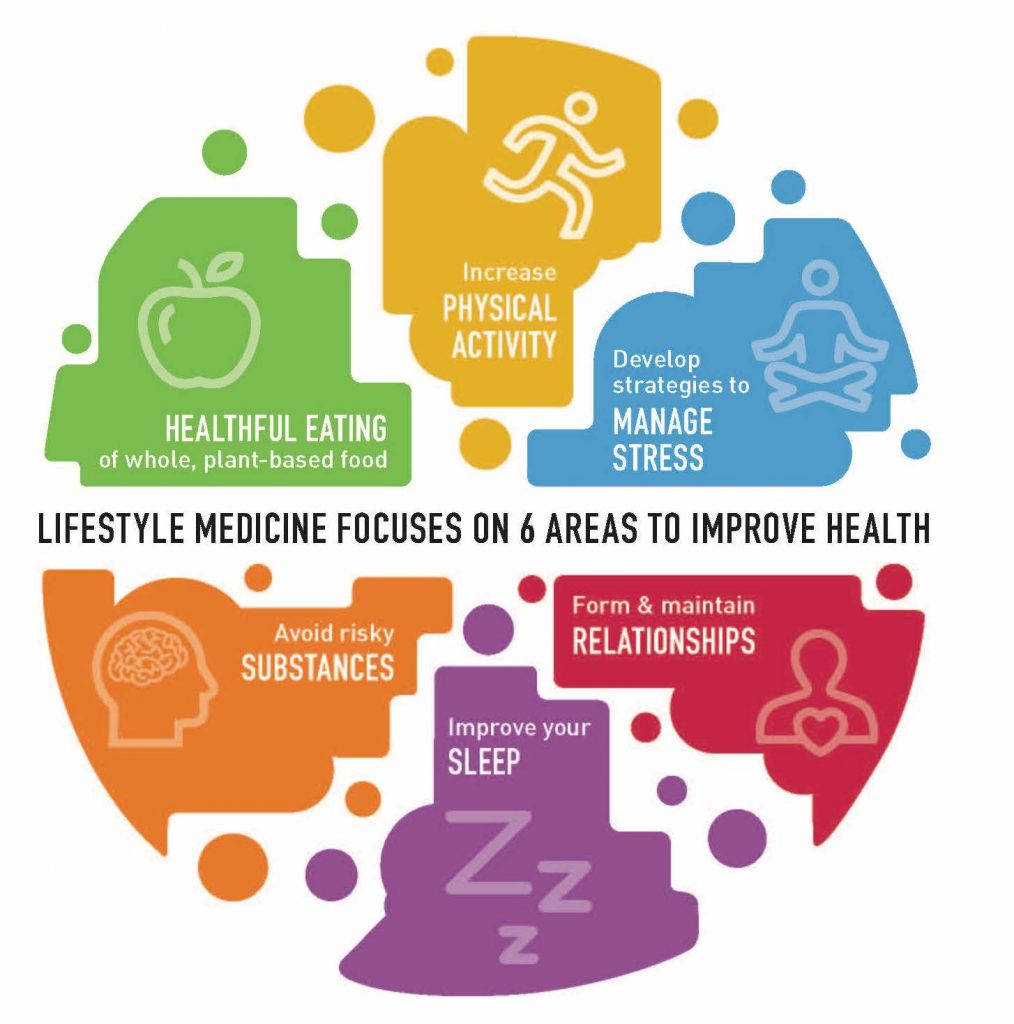
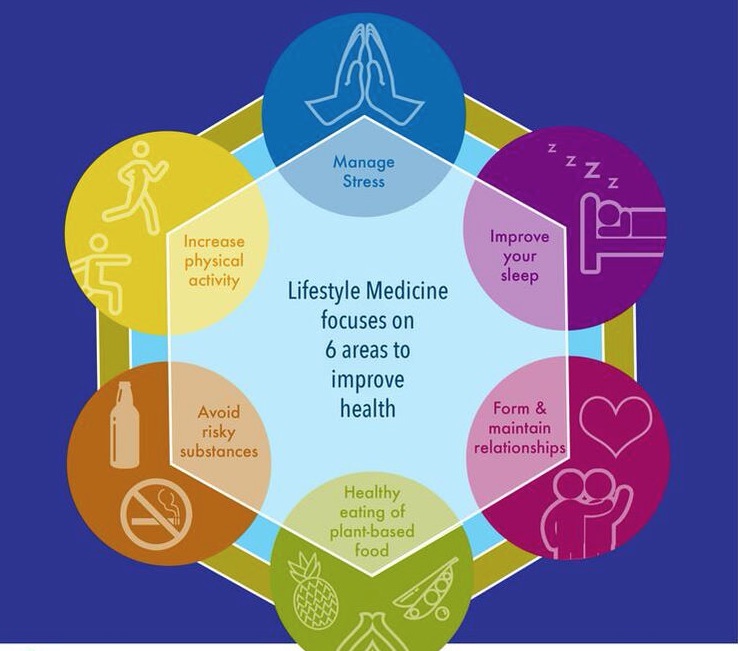
lifestyle medicine principle
Trauma Informed Lifestyle Medicine Model
There is nothing simple when it comes to anything about human beings, our behaviour, our brains, our cells, our systems, our diets and our diseases. Everything is complex and involves complex interactions implicit and explicit. The current way of thinking about disease, looking at disease and attempting to treat disease or even prevent disease is a reductionist model. When something is reduced it is narrow and simplistic which can be manualised and systematised but this approach looses sight of the bigger picture, the nuances, the complex interplays of body and environment and absolutely the root causes of the illness. A problem can not be addressed and solved without understanding all the possible factors involved in the problem. A trauma informed lifestyle medicine approach is a multi-disciplined consilient view of a client and their presentations, our approach is influenced by systems medicine and functional medicine but differs in our much greater focus on lifestyle, childhood adversity and quality of relationships which is to understand that the body is a system of complex systems which involve numerous complex processes, pathways, genetic expressions upregulated and down regulated sensing internal and external environments influenced by perceptions and previous experiences and the stressed or safety status of the nervous system via neuroception, and that all of this is much more shaped by childhood experience and relationships than any other factor thus the same is true for its treatment. A true healthcare approach must incorporate this consilient view and include models such as polyvagal theory, attachment theory, cell danger response theory and functional medicine, lifestyle medicine and culinary medicine. This is the work that we do at The Trauma Recovery Institute and this is what the course is based on.
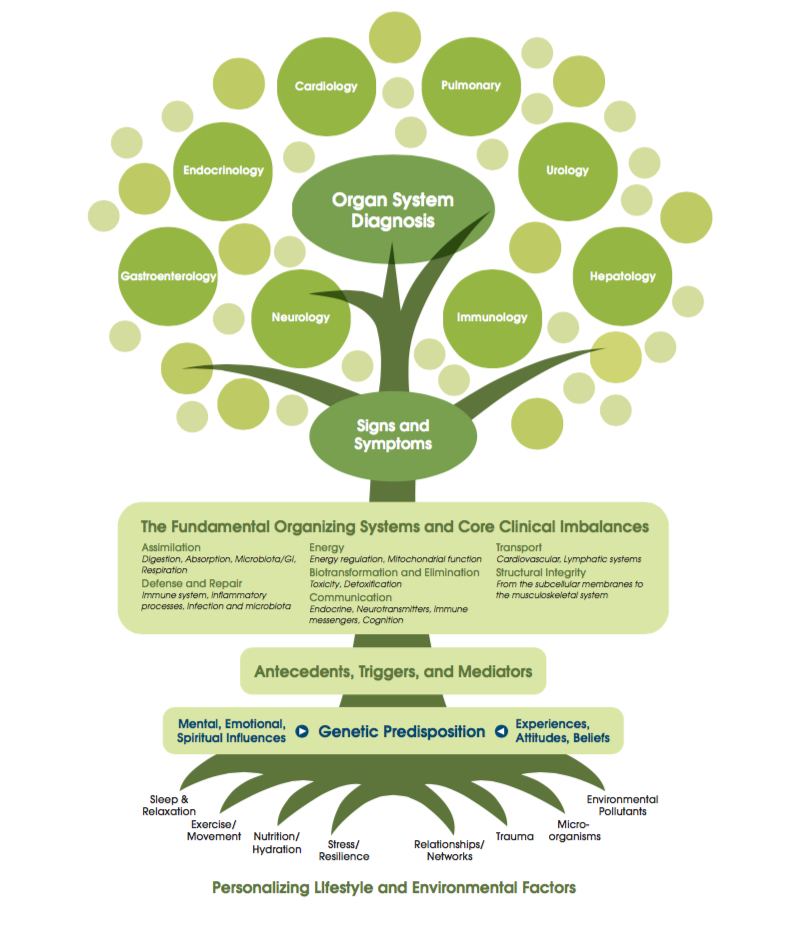
Chronic diseases are a consequence of interactions between a body and genome with the environment, including lifestyle and other risk/protective factors, throughout a life. In the clinic, these diseases express themselves often through comorbidities, whereas at the molecular and cell levels, most probably identifiable specific mechanisms and their alterations are responsible for a loss of physiological function through the age of the body. Biological complexity has forced molecular and cell biology into reduction and contextualization, with an ever-increasing degree of specialization. What is frequently lost or forgotten along this road of reduction, contextualization, and specialization is that the body is a system of systems with complex pathways and processes all speaking to each other and influencing each other in negative and positive cascades. Systems biology has taught us several lessons of which the following are of central importance : (i) many diseases have their origin in cellular malfunction, requiring a deep understanding of the mechanisms underlying cell functions; (ii) the emergence of diseases is a nonlinear dynamical phenomenon, requiring quantitative time-resolved monitoring of key biological parameters at the molecular, cellular, and physiological levels. Lifestyle Medicine is Preventive Medicine which we define as a comprehensive multidiscipline scientific approach to decreasing disease risk and illness burden by utilising lifestyle interventions such as plant based nutrition using culinary medicine approach, physical activity, stress reduction and management according to polyvagal principles, sleep hygiene, development and maintenance of healthy reciprocal relationships, including daily play and laughter, smoking cessation, and avoidance of other dangerous substances such as processed foods, sugar and alcohol.

The Relationship is the Therapy - The Therapeutic Alliance & Romantic Relationship
The Unconscious Contract
When we meet our partners, we make an unconscious contract to help each other resolve emotional injuries of the past , we unconsciously pick or hire the perfect person to trigger this stored painful memory of our past , it is for this exact reason we have come together . Relationships are not a problem to be solved but an adventure to be embraced. Conflict is a gift to be unpacked , to embrace, an opportunity to grow , resolve and mature . Conflict can not be resolved at the level with which it was created. We hire the person in our life who is most compatible to help us resolve what is unresolved from our childhood. Our relationship lives in the space between us and it is sacred . This becomes the playground for our children . When there are only two options , take the third option ! Keep the space between you safe and sacred . Honour the space between you , by visiting the other by crossing the bridge . Cross the bridge with an open mind to learn , with curiosity and compassion , leave behind your hurt and trauma. Crossing the bridge is becoming completely present with your partner, listening without interruption, defensiveness or judgement, holding an unconditional space for your partner to share.
The Premise of Trauma Informed Relational Model (TIRM)
- The Romantic Bond is the completion of what is unresolved / un repaired in the parental bond. Therefore the relationship is the therapy.
- We come together to complete , reenacting traumatic or adverse events so that awareness can be brought to a reemerging dynamic or feeling state in an effort for it to be healed, we do this through conflict and repair . This is the very purpose of the relationship.
- We strive to provide corrective emotional healing experiences for each other. Allowing each other into our internal world, sharing love maps and continuous invitations.
- The greater the childhood trauma and neglect, the uglier the conflict and reenactment will be.
- Conflict and repair is a necessary psychological, metabolic and neurological process which is an adaptive and hormetic response. Avoiding this process can create disease, which is driven by chronic States of sympathetic activation (fight/flight) or dorsal vagal activation (shut down) of the nervous system and stuck unrepaired cell danger response.
- Feelings are not facts, but they are real and meaningful and most likely familiar.
- Co regulation produces safety, down regulating outside the relationship can erode safety.
- Manage the masculine and feminine energies. The feminine needs safety and to feel priority , the masculine needs goals and purpose and accomplishment . Help the masculine be good at the relationship and that’s where he will focus. Lift the feminine up, help her feel safe and she will bring a huge amount of love and nurturing to the relationship.
- Compassionate curiosity is an important muscle to exercise.
- Use the 7 principles as a way to frame and repair conflicts.
Seven principles for Co Creating a Conscious Relationship with The Ultimate Relationship Program
- The relationship lives in the space between us.
- The emotional charged part of your partner is the child in them trying to tell their story , allow each other to tell that story by crossing the bridge.
- We are energy that can be positive and negative , be aware of this energy by not making the space toxic .
- When our partners exhibits bewildering behaviour , it is a cry for help from the child within them , the behaviour is a protection , get to know each other's cry for help .
- The stretching principle is based on the idea that every frustration in the relationship is a gift to be unpacked. Thank your partner for this opportunity to grow.
- Release joy into the relationship. Play, joy and fun are all essential ingredients for connection and repairing any disconnection in the relationship, it is also important to direct our passion into the relationship otherwise these passion will be redirected outside the relationship and we will begin to feel the relationship is no longer working.
- Create a compelling dream together as a couple. Define the relationship, be specic about goals and plans short term and long term. when we are specific we deirect enegry towards attracting and achieving our dreams and goals.
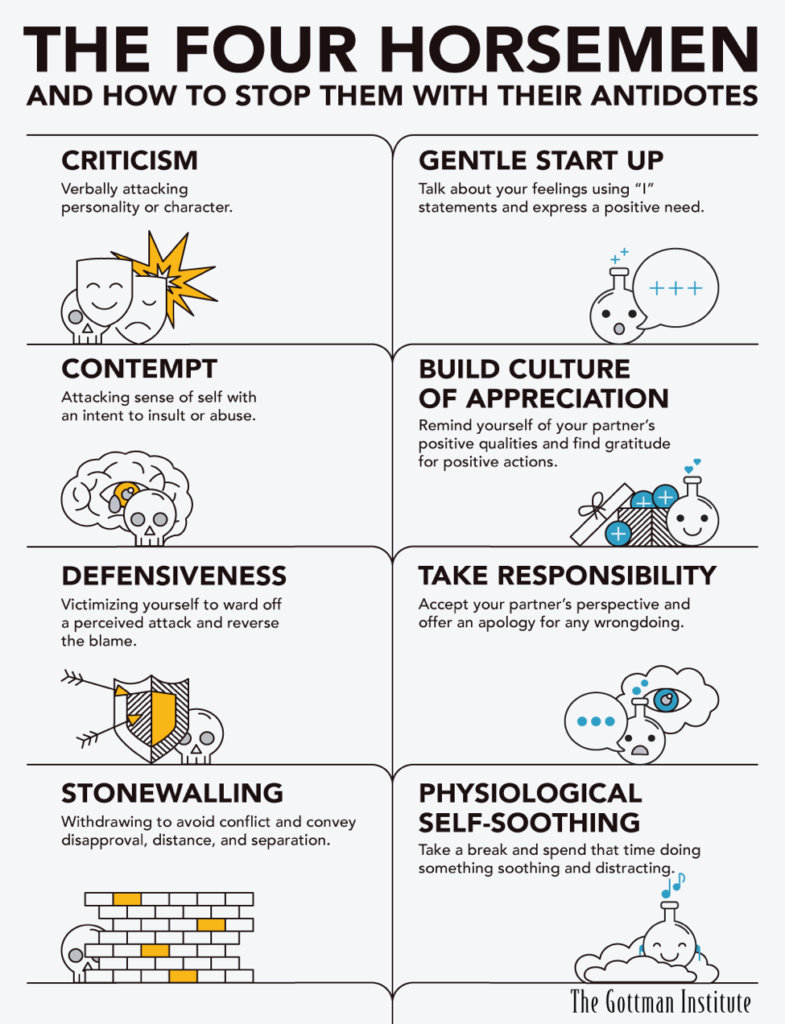
1. Criticism
Criticizing your partner is different than offering a critique or voicing a complaint. The latter two are about specific issues, whereas the former is an ad hominem attack. It is an attack on your partner at the core of their character. In effect, you are dismantling their whole being when you criticize. The important thing is to learn the difference between expressing a complaint and criticizing:
- Complaint: “I was scared when you were running late and didn’t call me. I thought we had agreed that we would do that for each other.”
- Criticism: “You never think about how your behavior is affecting other people. I don’t believe you are that forgetful, you’re just selfish. You never think of others! You never think of me!”
If you find that you and your partner are critical of each other, don’t assume your relationship is doomed to fail. The problem with criticism is that, when it becomes pervasive, it paves the way for the other, far deadlier horsemen to follow. It makes the victim feel assaulted, rejected, and hurt, and often causes the perpetrator and victim to fall into an escalating pattern where the first horseman reappears with greater and greater frequency and intensity, which eventually leads to contempt.
2. Contempt
When we communicate in this state, we are truly mean—we treat others with disrespect, mock them with sarcasm, ridicule, call them names, and mimic or use body language such as eye-rolling or scoffing. The target of contempt is made to feel despised and worthless. Contempt goes far beyond criticism. While criticism attacks your partner’s character, contempt assumes a position of moral superiority over them:
Research even shows that couples that are contemptuous of each other are more likely to suffer from infectious illness (colds, the flu, etc.) than others due to weakened immune systems! Contempt is fueled by long-simmering negative thoughts about the partner—which come to a head when the perpetrator attacks the accused from a position of relative superiority. Most importantly, contempt is the single greatest predictor of divorce. It must be eliminated.
3. Defensiveness
Defensiveness is typically a response to criticism. We’ve all been defensive, and this horseman is nearly omnipresent when relationships are on the rocks. When we feel unjustly accused, we fish for excuses and play the innocent victim so that our partner will back off. Unfortunately, this strategy is almost never successful. Our excuses just tell our partner that we don’t take their concerns seriously and that we won’t take responsibility for our mistakes:
- Question: “Did you call Betty and Ralph to let them know that we’re not coming tonight as you promised this morning?”
- Defensive response: “I was just too darn busy today. As a matter of fact, you know just how busy my schedule was. Why didn’t you just do it?”
This partner not only responds defensively, but they reverse blame in an attempt to make it the other partner’s fault. Instead, a non-defensive response can express acceptance of responsibility, admission of fault, and understanding of your partner’s perspective:
Although it is perfectly understandable to defend yourself if you’re stressed out and feeling attacked, this approach will not have the desired effect. Defensiveness will only escalate the conflict if the critical spouse does not back down or apologize. This is because defensiveness is really a way of blaming your partner, and it won’t allow for healthy conflict management.
4. Stonewalling
Stonewalling is usually a response to contempt. Stonewalling occurs when the listener withdraws from the interaction, shuts down, and simply stops responding to their partner. Rather than confronting the issues with their partner, people who stonewall can make evasive maneuvers such as tuning out, turning away, acting busy, or engaging in obsessive or distracting behaviors. It takes time for the negativity created by the first three horsemen to become overwhelming enough that stonewalling becomes an understandable “out,” but when it does, it frequently becomes a bad habit. And unfortunately, stonewalling isn’t easy to stop. It is a result of feeling physiologically flooded, and when we stonewall, we may not even be in a physiological state where we can discuss things rationally. If you feel like you’re stonewalling during a conflict, stop the discussion and ask your partner to take a break:
Then take 20 minutes to do something alone that soothes you—read a book or magazine, take a walk, go for a run, really, just do anything that helps to stop feeling flooded—and then return to the conversation once you feel ready.
If You Want to Change the World, Love a Woman - Lisa Citore
If you want to change the world… love a woman-really love her. Find the one who calls to your soul, who doesn’t make sense. Throw away your check list and put your ear to her heart and listen. Hear the names, the prayers, the songs of every living thing- every winged one, every furry and scaled one, every underground and underwater one, every green and flowering one, every not yet born and dying one…
Hear their melancholy praises back to the One who gave them life. If you haven’t heard your own name yet, you haven’t listened long enough. If your eyes aren’t filled with tears, if you aren’t bowing at her feet, you haven’t ever grieved having almost lost her.
If you want to change the world… love a woman-one woman beyond yourself, beyond desire and reason, beyond your male preferences for youth, beauty and variety and all your superficial concepts of freedom.
We have given ourselves so many choices we have forgotten that true liberation comes from standing in the middle of the soul’s fire and burning through our resistance to Love.
There is only one Goddess. Look into Her eyes and see-really see if she is the one to bring the axe to your head. If not, walk away. Right now. Don’t waste time “trying.” Know that your decision has nothing to do with her because ultimately it’s not with who, but when we choose to surrender.
If you want to change the world… love a woman. Love her for life-beyond your fear of death, beyond your fear of being manipulated by the Mother inside your head. Don’t tell her you’re willing to die for her. Say you’re willing to LIVE with her, plant trees with her and watch them grow. Be her hero by telling her how beautiful she is in her vulnerable majesty, by helping her to remember every day that she IS Goddess through your adoration and devotion.
If you want to change the world… love a woman in all her faces, through all her seasons and she will heal you of your schizophrenia- your double-mindedness and half-heartedness which keeps your Spirit and body separate- which keeps you alone and always looking outside your Self for something to make your life worth living. There will always be another woman. Soon the new shiny one will become the old dull one and you’ll grow restless again, trading in women like cars, trading in the Goddess for the latest object of your desire.
Man doesn’t need any more choices. What man needs is Woman, the Way of the Feminine, of Patience and Compassion, non-seeking, non-doing, of breathing in one place and sinking deep intertwining roots strong enough to hold the Earth together while she shakes off the cement and steel from her skin.
If you want to change the world… love a woman, just one woman . Love and protect her as if she is the last holy vessel. Love her through her fear of abandonment which she has been holding for all of humanity. No, the wound is not hers to heal alone. No, she is not weak in her codependence.
If you want to change the world… love a woman all the way through until she believes you, until her instincts, her visions, her voice, her art, her passion, her wildness have returned to her- until she is a force of love more powerful than all the political media demons who seek to devalue and destroy her.
If you want to change the world, lay down your causes, your guns and protest signs. Lay down your inner war, your righteous anger and love a woman… beyond all of your striving for greatness, beyond your tenacious quest for enlightenment.
The holy grail stands before you if you would only take her in your arms and let go of searching for something beyond this intimacy.
What if peace is a dream which can only be re-membered through the heart of Woman? What if a man’s love for Woman, the Way of the Feminine is the key to opening Her heart?
If you want to change the world…love a woman to the depths of your shadow, to the highest reaches of your Being, back to the Garden where you first met her, to the gateway of the rainbow realm where you walk through together as Light as One, to the point of no return, to the ends and the beginning of a new Earth.
If you want to change the world, love a Woman, if you want to become powerful… love a woman, if you want to heal… love a woman, if you want success…. Love a woman. Become the richest and most powerful man and Love a woman.


Transference at The Trauma Recovery Institute

“Transference is also an assimilation of what might happen in the future if we act on the impulse in the here and now, also as mirroring of the past” Such reenactments are crucial disclosures about un-integrated, un-symbolized unformulated experience. Understanding the unconscious communication within a reenactment is often pivotal point in the therapeutic relationship with a traumatized adult, in particular a sexually abused adult. Seen in this light, enactment is a way for a client to allow himself/herself to be known by co constructing, with the therapist, a means of living out a new, less disabling version of the original trauma. In this co construction, cognitive symbolization of trauma occurs when the trauma is reenacted within a relationship, reproducing the original interpersonal context but not leading to the original outcome. Once this happens, dissociated experience is transformed to internal conflict and human relatedness, which are more available for verbal consideration in psychotherapy or and in the relationship. By working through reenactments in the relationship with a skilled right brain focussed psychotherapist thus gradually obtaining access to the various multiple dissociated self-states which is liberating but also allows us to experience a much richer fuller life experience and helps us to love deeply. The exploration of the reenactment is embedded in the therapeutic relationship.
Therapist and client forming the safe therapeutic alliance becomes both the magnet that draws out the reenactment and the architect of a transitional arena in which the client experiences of self and other can be reconfigured in more harmonious ways In seeing the therapeutic relationship this way, thus therapy may rely upon the hope that therapist and client together will become enmeshed in complicated reenactments of early unformulated experiences with significant others, that can shed light upon our current interpersonal and intrapsychic difficulties by reopening them in the therapeutic relationship, prematurely foreclosed areas of experience. If the reenactment is to be integrated as other than the original trauma, however something essentially different must happen which we call a corrective emotional experience. The relational models of transference and countertransference {Relational Conflict} are reenactments of different aspects of the dissociated relationships involved in victimization by a parent or a caregiver. The more trauma experienced in childhood, the more complicated the conflict and the greater difficultly with understanding the symbolism of the reenactment and therefore the repair. Often abusive aggressive and painful reenactments are an inevitable part of the relationship with an abused especially sexually abused person and also an inevitable part of the working through in a therapeutic relationship with a sexually abused client.
The being who is the object of his own reflection, in consequence of that very doubling back upon himself, becomes in a flash able to raise himself into a new sphere. In reality, another world is born.
Pierre Teilhard De Chardin
Relational Conflict can be another way of framing Transference – countertransference reenactments in relationships which are vehicles for communication to each other about the internal relational experience of the child as he/she was being abused. As such they are powerful tools but they are also forceful and often coercive catalysts in the relationship. Reenactment compels the therapist to experience the client’s original reactions to abuse, reactions that are dissociated aftermath to a deeply traumatic childhood experience. To heal the client of the trauma, the therapist must experience that trauma in some way. The reenactment may be just symbolic of the abuse but the feelings engendered in the relationship are very real. These may include helplessness, impotence, rage, inadequacy, shame, guilt, idealisation, omnipotence, overstimulation, humiliation, torture and fear, all internal states with which the client is very familiar.
Thus helping the client whose relationships and personalities are organised by dissociation involves a challenge psychological encounter with the trauma that caused the dissociation in the first place. We can can easily feel traumatised under such circumstances as strong reenactments and conflict in the relationship, yet it is important to remember that neither reenactments nor conflict reactions to them are necessarily mistakes rather they are unavoidable phases in the working through of traumatised dissociated people or unavoidable phases in the working through of a therapeutic alliance and relationship with a traumatised dissociated client. A large premise of interpersonal neurobiology is that the brain is also pursuing healing. So we are compelled to reenact creating conflict in order to invoke a repair. Rupture will and should happen but healing will not happen with our repair. “The road to an increasingly secure relationship is usually and exceedingly rocky one precisely because the defenses we use to avoid the painful past often wind up provoking it’s recreation in the present.” It has commonly been noted that a previously abused or neglected child who is now an adult in relationship tends to identify with their abusers and then to be transferentially abusive/neglectful to their partners within the interpersonal/romantic relationship. In doing this they are repeating with their partner what happened to them as children. The abuse-victim relational configuration is particularly upsetting conflict within a romantic relationship because of its ubiquitous intense transference and countertransference enactments.
Interactive psychobiological regulation provides the relational context under which the client can safely contact, describe and eventually regulate inner experience. It is the client's experience of empowering action in the context of safety provided by a background of the empathic clinician's psychobiologically attuned interactive affect regulation that helps effect change. This form of presence to right brain affect regulation is critical for change process in psychotherapy.
The Trauma Recovery Institute
Resourcing Activities





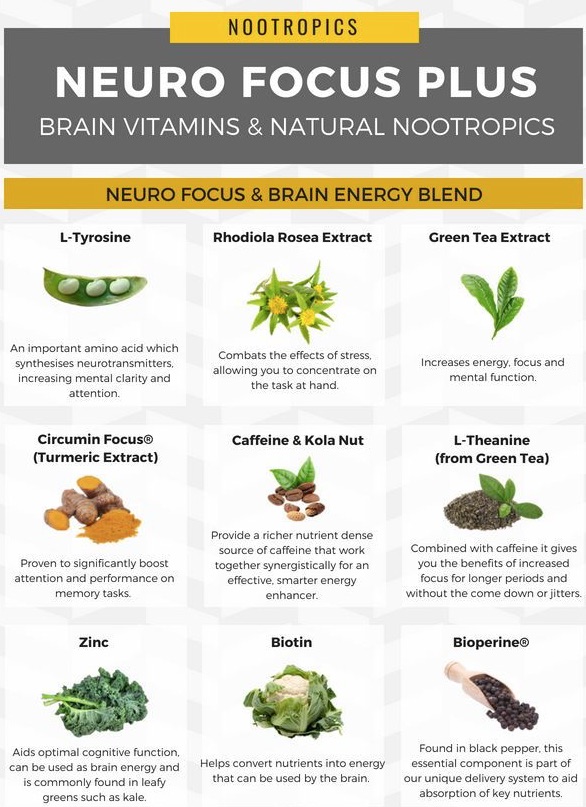
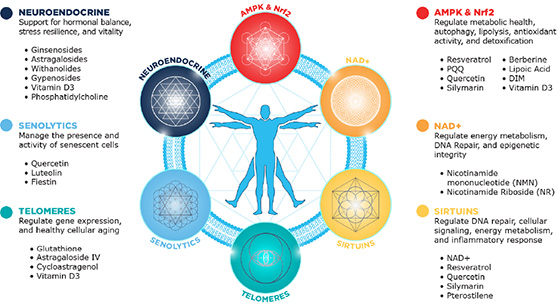
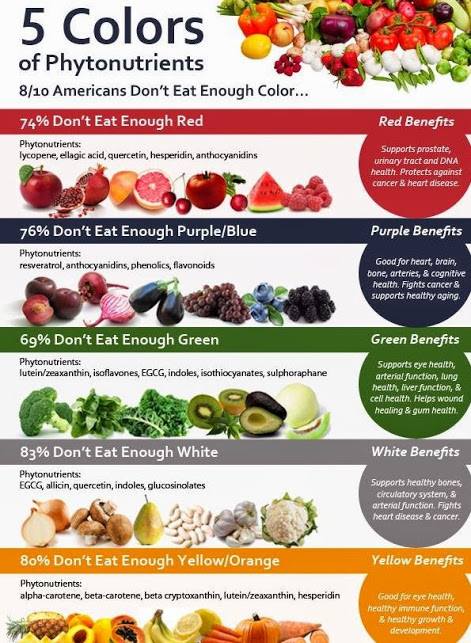
Supplement & Detoxification Support For Chronic Stress, inflammation, Anxiety & PTSD