02 Jan Treating Complex Trauma at The Trauma Recovery Institute
Defining Trauma
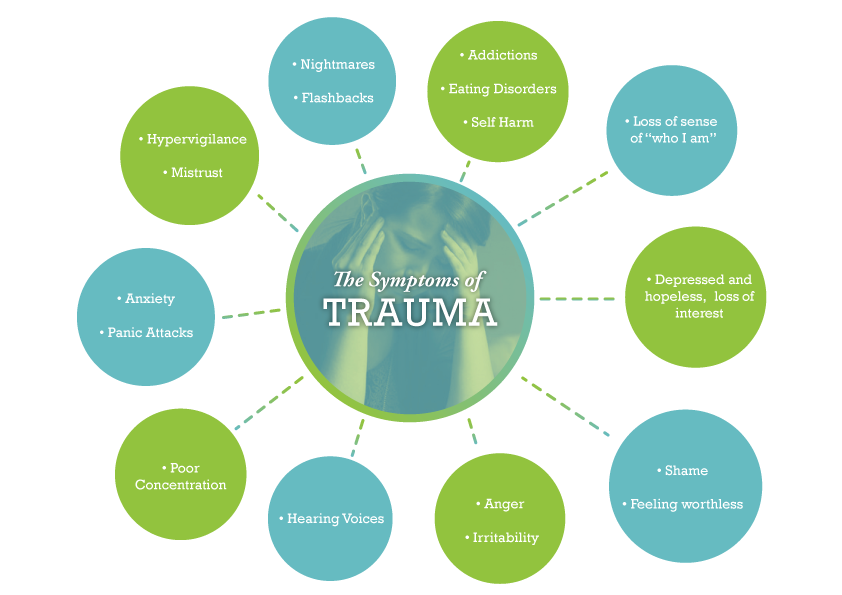
The prevailing definition of trauma has been that psychological trauma is a response to an event that a person finds highly stressful. Examples include being in a war zone, a natural disaster, or a serious car accident. We now understand so much more about trauma, its definition and implications and it seems trauma is much broader and more complex than once appreciated, perhaps best seen as a spectrum including adverse childhood experiences, neglect, sexual abuse, violence, bullying and ofcourse attachment trauma. As a trauma specialist at The Trauma Recovery Institute, I propose that in-fact most of us have experienced some form of trauma or/and adversity growing up, evidenced by the prevalence in our society of addictions to food, drugs and alcohol, our difficulty as a society to maintain healthy long term romantic relationships and our overwhelming health crisis due to poor lifestyle choices. Once seen as all very separate societal challenges, now it is difficult to separate any of the above from adverse childhood experiences. Our childhood is the critical period for brain development which is shaped by experience, experiences become our biology and so dictates how we engage in the world later on, largely governing the choices we make, the relationships we enter into or choose not to, how skilled we are in those relationships including romantic and parental and our relationship to our physical and mental health. A rather elegant way of describing trauma or at least traumatic events is things that happened that should never have happened and things that did not happen which should have happened in cases such as childhood neglect. In the field of traumatology there is a move away from labelling an event as trauma and even the story created out of an event and moving towards seeing trauma as the body’s response to an event or events, in other words, trauma is what lives on in the body/mind and nervous system long after a traumatic event or period. Complex trauma is now understood to be attachment trauma known as disorganised attachment followed by subsequent traumatic events.
The effect of the experience of trauma over the life span lays the seeds for most chronic, poorly understood disease processes that defy explanation by our current concepts of health and disease. These chronic diseases make up the majority of symptoms for which patients present to doctor’s offices. The brain, mind, and body exist on a continuum, wherein sensory input from the body shapes and changes the structure and function of the brain, which concurrently shapes and alters the body in all of its parts — particularly those that provided the sensory input to the brain. The brain and body are intimately inter- related rather than two distinct parts of the greater whole. These two parts of the continuum form a dynamically changing nervous system, constantly and reciprocally adapting based on the influence of the other.
The mind is a receptacle for perceptual experience, including body sensations or feelings, and the positive or negative emotions that are related to that information. The mind is based on brain activity and is the conscious manifestation of what we sense and feel based on the dynamic interaction of the brain / body. Trauma can be conceptualized as stemming from a failure of the natural physiological activation and hormonal secretions to organize an effective response to threat. Rather than producing a successful fight or flight response the organism becomes immobilized. Probably the best animal model for this phenomenon is that of ‘inescapable shock,” in which creatures are tortured without being unable to do anything to affect the outcome of events. The resulting failure to fight or flight, that is, the physical immobilization (the freeze response), becomes a conditioned behavioral response. The psychobiology of early childhood development involving maturation of orbitofrontal and limbic structures is based on reciprocal experiences with the caregiver we call attunement, the nonverbal reciprocal exchange of safety cues between mother and child. Dysfunctional associations in this dyadic relationship result in permanent physicochemical and anatomical changes, which have implications for personality development as well as for a wide variety of clinical manifestations. An intimate relationship may exist, with negative child/care giver interaction leading to a state of persisting hypertonicity of the sympathetic and parasympathetic systems that may profoundly affect the arousal state of the developing child. Sustained hyperarousal in these children may markedly affect behavioral and characterological development.
Many traumatized children and adults, confronted with chronically overwhelming emotions, lose their capacity to use emotions as guides for effective action. They often do not recognize what they are feeling and fail to mount an appropriate response. This phenomenon is called alexithymia, an inability to identify the meaning of physical sensations and muscle activation. Failure to recognize what is going on causes them to be out of touch with their needs, and, as a consequence, they are unable to take care of them. This inability to correctly identify sensations, emotions, and physical states often extends itself to having difficulty appreciating the emotional states and needs of those around them. Unable to gauge and modulate their own internal states they habitually collapse in the face of threat, or lash out in response to minor irritations. Dissociation and/or Futility become the hallmark of daily life.


Trauma Recovery at The Trauma Recovery Institute
TRAUMA & LEARNED RESPONSES
Traumatic life experiences often contribute to learned habits of movement and posture that reflect the self-protective movement patterns associated with those threats. Many of these trauma-related movement patterns affect the way that we move, sit and stand. They may lead to patterns of movement and posture that are abnormal and they may inhibit our normal coordination and our learning of other desirable motor skills.Self-protective movement and postural patterns of the experienced trauma are stored in the brain and the body’s survival memory. These learned dysfunctional patterns persist because they are, in a metaphorical sense, necessary for defense against future threats similar to those that elicited the defense in the first place. If traumatic memories are implanted in the brain, internal cues (such as dreams, imagined scenarios, and memories) as well as sensory information from the external environment will evoke motor, autonomic, somatic, and visceral responses to a perceived threat. This process is almost entirely unconscious and occurs typically before any conscious recognition or awareness. Using the term ‘psychological’ as opposed to ‘physical’ to explain a physical symptom or somatic feeling state or emotional event defies the obvious – that all perceptions, thoughts, symbols, or experiences have a physiological basis within the mind / body continuum.
Dynamic Psychosocialsomatic Psychotherapy
is grounded in models such as affect regulation theory, an interpersonal neurobiological model of emotional and social development from early human beginnings and across the lifespan, attachment research, polyvagal theory, traumatology and interpersonal neurobiology. Drawing upon these various scientific and clinical disciplines, our trauma recovery work describes how the structure and function of the right mind and brain are indelibly shaped by experiences, especially those embedded in emotional relationships, and how communicating right brains align and synchronize their neural activities with other right brains. These experiences of interpersonal synchrony are a central focus of Psychosocialsomatic Psychotherapy. At The Trauma Recovery Institute we attempt to get to the root of your life challenging symptoms, discomfort, illness and maladaptive behaviours. This is not another talk therapy, although talking is certainly a part of psychotherapy, it is not the central feature of focus, talking in this context is about communicating body awareness, building therapeutic alliance, challenging internal object relations, investigating transferences etc. We offer a broad multi-disciplined, somatic orientated, polyvagal informed right brain to right brain approach to treating trauma. We also specialise in personality disorders & complex trauma. Our approach brings focus on the brain, body, mind, diet, lifestyle, relationships and most importantly the nervous system of which traumatic experiences have greatly shaped thus priming a predisposition of subsequent adversity. The definition of a traumatic experience is an experience or experiences that overwhlem our capacity to cope. Trauma effects all areas of the brain and all bodily systems often manifesting as cancer, IBS and a host of other chronic illnesses and pain syndromes which can not be otherwise explained.
At The Trauma Recovery Institute We Endeavour
- to co-create an interpersonally synchronized right brain-to-right brain emotional dialogue beneath the words with clients
- to empathically receive the client’s rapid implicit (unconscious) nonverbal communications in synchronized mutual regressions
- to sensitively monitor very slight changes in the other’s emotional expressions
- to intuitively track physiological variations in the patient’s emotional prosody, facial expressions, and gestures
- to interoceptively read one’s own physiological autonomic responses to the client’s emotional communications
- to transiently shift from the verbal left into the nonverbal right brain and the deeper core of the personality
- to co-create a relational context of implicit safety and trust with the client
- to be able to work with strong, traumatic affect and relational trauma, typically found in personality and psychiatric disorders
- to engage in stressful dyadic transference-countertransference and rupture and repair transactions
- to be intuitively aware of one’s own spontaneous bodily-based subjective and intersubjective experience
- to offer well-timed interventions and interpretations that can impact the client’s unconscious levels
- to interactively regulate the patient’s dysregulated affective states, across a spectrum of psychopathologies.
At The Trauma Recovery Institute We Focus
on how to work more directly and effectively with bodily-based emotions, unconscious affect and transference – countertransference within the therapeutic relationship, especially in “heightened affective moments” of the session. Attention is also placed upon working with the defenses of right brain dissociation and left brain repression that blot out strong emotions from consciousness. This central focus on right (and not left) brain affect regulation in the co-created psychotherapy relationship shifts the clinical focus from a reasoned, coherent cognitive narrative to a spontaneous emotion-laden conversation. In this manner the clinical emphasis moves from objective cognitive insight to the subjective change mechanisms embedded in the emotional attachment bond of the therapeutic relationship itself. Trauma Recovery is a complex pursuit and due to trauma and neglect’s impact on all bodily systems, any approach to address the presenting symptoms will be an oversimplified model, therefore we must approach trauma with a multidisciplinary approach on top of cultivating presence and establishing a strong therapeutic alliance with our clients. Modules of treatments such as SE, EMDR, Neurofeedback etc may be helpful adjuncts but they are way too simplified to be effective treatment for trauma, complex trauma and the presenting symptoms of trauma and neglect. The right brain implicit self represents the biological substrate of the human unconscious mind and is intimately involved in the processing of bodily based affective information associated with various motivational states. The survival functions of the right hemisphere, the lo- cus of the emotional brain, are dominant in relational contexts at all stages of the lifespan, including the intimate context of psychotherapy. The central focus of the psychotherapeutic encounter is to appreciate the client’s motivation, we need to discern the emotional experience he or she seeks. At times, the goal sought will be self- evident to client and [therapist]. At other times, the goal will lie out of awareness and will be difficult to ascertain. The golden thread in assessing motivation lies in discovering the affect being sought in conjunction with the behavior being investigated. In other words, understanding the need underpinning the behaviour, the corrective emotional experience so to speak. The right hemisphere is dominant for the recognition of emotions, the expression of spontaneous and intense emotions, and the nonverbal communication of emotions. The central role of this hemisphere in survival functions is that the right hemisphere operates a distributed network for rapid responding to danger and other urgent problems. It preferentially processes environ- mental challenge, stress and pain and manages self-protective responses such as avoidance and escape. Emotionality is thus the right brain’s “red phone,” compelling the mind to handle urgent matters without delay. Neurobiological studies also demonstrate that the right cortical hemisphere is centrally involved in “the processing of self-images, at least when self-images are not consciously perceived. Deep psychotherapeutic changes alter not only conscious but unconscious self-image associated with nonconscious internal working models of attachment. Both unconscious negative emotions and unconscious self-images are important elements of the psychotherapy process, especially with the more severe self pathologies. Thus, the essential roles of the right brain in the unconscious processing of emotional stimuli and in emotional communication are directly relevant to recent clinical models of an affective unconscious and a relational unconscious, whereby one unconscious mind communicates with another unconscious mind such at that with the therapeutic alliance.
Why Not Talk Therapy
There is much confusion regarding talk therapy which I would like to offer some clarification on. Many trauma researchers including myself over a number of years have suggested that talk therapy does not work or talk therapy is not enough to address the trauma because the trauma is often stored in the body. There has been a host of fantastic published work showing that in-fact trauma is stored in the body. It is also well documented and I concur from my many years in clinical practise that recalling traumatic events and sharing the story of the trauma offers very little relief of trauma symptoms. Having said that any therapy that offers trauma treatment without talking certainly will not address trauma either and will most likely be an extraordinarly over simplified treatment or may infect be retraumatising particularly if involving touch.The body must come into the therapy but talk must be present too. The origins of talk therapy come from freud’s talking cure therapy of free association. Freud was less interested in the unpredicictibility of emotions and instead relied on the thoughts of his patients. Allowing patients to simply talk in order to relieve symptoms. There are other forms of talk therapy that are more modern such as grief counselling and other forms of counselling and cognitive behavioural therapy. In any trauma informed psychotherapeutic treatment of trauma there will indeed be talking but it does not take centre stage, it is just one part of the therapeutic alliance and one part of top down modality in a multidisciplinary approach. Trauma is very complex and an effective treatment model must be as broad as possible and multidisciplinary.


No Comments